A POOLED DATA ANALYSIS OF TWELVE CLINICAL TRIALS OF FONDAZIONE ITALIANA LINFOMI (FIL): KHORANA SCORE AND HISTOTYPE PREDICT THE INCIDENCE OF EARLY VENOUS THROMBOEMBOLISM (VTE) IN NON HODGKIN LYMPHOMA
(Abstract release date: 05/19/16)
EHA Library. Santi R. 06/09/16; 132500; E951

Dr. Roberto Santi
Contributions
Contributions
Abstract
Abstract: E951
Type: Eposter Presentation
Background
Recent studies show that the risk of VTE in Non Hodgkin Lymphoma (NHL) patients (pts) is similar to that observed in high risk solid tumors (i.e. pancreatic, ovarian cancer). VTE in NHL occurs in most cases within 3 months from diagnosis and can have substantial impact on treatment delivery and outcome as well as on quality of life. However few data are available on potential predictors.
Aims
To better clarify the epidemiology of early (within 6 months from treatment start) VTE in NHL pts we conducted a pooled data analysis of 12 clinical trials from FIL. Our analysis included basic demographic features, lymphoma-related characteristics as well as the Khorana score KS (based on histology, body mass index BMI, platelets count PLTs, white blood cells count WBC and hemoglobin values Hb) which is extensively used in solid tumors to predict VTE risk.
Methods
From Jan. 2010 to Dec. 2014 all pts with B-cell NHL enrolled in prospective clinical trials from FIL for frontline treatment were included. For 9 studies the study period included the entire trial population. The analysis was conducted based on CRFs as well as pharmacovigilance reports. VTE definition and grading was stated according to standard criteria of toxicity (CTCAE V4.0). Cumulative incidence of VTE from study enrollment was estimated using the method described by Gooley et al. accounting for death from any causes as a competing risk. The Fine & Gray survival model was used to identify predictors of VTE among NHL pts. Factors predicting the grade of VTE were investigated using an ordinal logistic regression model. This pooled data analysis was approved by local IRB.
Results
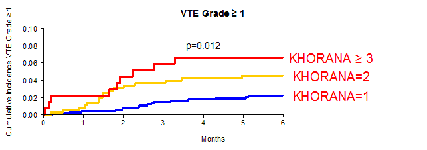
Overall, 1717 pts belonging to 12 studies were evaluated. 8 studies were phase I/II or II (25% of pts) and 4 phase III (75% of pts). M/F ratio was 1.41, median age was 57 (IQ range IQR 49-66). Histologies were: diffuse large B-cell lymphoma DLCL-B 34%, follicular lymphoma FL 41%, mantle cell lymphoma MCL 18%, other 6%. Median BMI was 25 (IQR 22-28). Median Hb, WBC and PLTs counts were 13g/dl (IQR 11.5-14.2), 7,1x10^9/l (IQR 5.6-10.3) and 224x10^9/l (IQR 169-298) respectively. In 1189 pts was assessed KS: 58% low risk, 30% intermediate risk, 12% high risk. Human erytropoetin support was given to 9% of pts. All pts received Rituximab. Planned therapeutic programs included autologous stem cells transplantation in 27% of pts, conventional chemotherapy in 67% and conventional chemotherapy plus lenalidomide in 6%. Overall 59 any grade VTE episodes occurred in 51 pts (2.9%), including 21 grade III-IV VTEs (18 pts). None was fatal. Median time from study enrollment to VTE was 63 days (IQR: 35-110). Considering death as a competitive event the 6 months cumulative incidence of VTE was 2,2% (95%IC: 1.1-3.3) in low risk, 4.5% (95%IC: 2.3-6.7) in intermediate and 6.6% (95%IC: 2.4-10.8) in high risk KS (p=0.012). KS was predictive also for grade III-IV VTEs as they were 0,7% (95%IC:0.1-1.4) in low risk and 2% (95%IC:0.8-3.3) in intermediate-high risk (p=0.048). Results were similar also after excluding lenalidomide containing studies.Fine and Gray multivariate analysis, adjusted for age and stage, showed that KS (intermediate risk adjHR=1.96; 95%IC: 0.84-4.56 and high risk adjHR=3.81; 95%IC: 1.51-9.58) and DLCL-B histotype (adjHR=2.58; 95%IC: 1.01-6.55) were independently associated to an increased risk of VTE. Moreover an ordinal logistical regression model indicated that the increase of 1 point in the KS resulted in an increased risk of VTE (OR=1.85; 95%CI: 1.23-2.79).
Conclusion
Our results suggest that DLCL-B hystotype and KS are predictors of VTE in NHL. The latter might become a simple and effective tool to assess the risk of VTE in NHL. Prospective validation including also pts not eligible for clinical trials is needed.
Session topic: E-poster
Keyword(s): Chemotherapy toxicity, Diffuse large B cell lymphoma, Thrombosis
Type: Eposter Presentation
Background
Recent studies show that the risk of VTE in Non Hodgkin Lymphoma (NHL) patients (pts) is similar to that observed in high risk solid tumors (i.e. pancreatic, ovarian cancer). VTE in NHL occurs in most cases within 3 months from diagnosis and can have substantial impact on treatment delivery and outcome as well as on quality of life. However few data are available on potential predictors.
Aims
To better clarify the epidemiology of early (within 6 months from treatment start) VTE in NHL pts we conducted a pooled data analysis of 12 clinical trials from FIL. Our analysis included basic demographic features, lymphoma-related characteristics as well as the Khorana score KS (based on histology, body mass index BMI, platelets count PLTs, white blood cells count WBC and hemoglobin values Hb) which is extensively used in solid tumors to predict VTE risk.
Methods
From Jan. 2010 to Dec. 2014 all pts with B-cell NHL enrolled in prospective clinical trials from FIL for frontline treatment were included. For 9 studies the study period included the entire trial population. The analysis was conducted based on CRFs as well as pharmacovigilance reports. VTE definition and grading was stated according to standard criteria of toxicity (CTCAE V4.0). Cumulative incidence of VTE from study enrollment was estimated using the method described by Gooley et al. accounting for death from any causes as a competing risk. The Fine & Gray survival model was used to identify predictors of VTE among NHL pts. Factors predicting the grade of VTE were investigated using an ordinal logistic regression model. This pooled data analysis was approved by local IRB.
Results
Overall, 1717 pts belonging to 12 studies were evaluated. 8 studies were phase I/II or II (25% of pts) and 4 phase III (75% of pts). M/F ratio was 1.41, median age was 57 (IQ range IQR 49-66). Histologies were: diffuse large B-cell lymphoma DLCL-B 34%, follicular lymphoma FL 41%, mantle cell lymphoma MCL 18%, other 6%. Median BMI was 25 (IQR 22-28). Median Hb, WBC and PLTs counts were 13g/dl (IQR 11.5-14.2), 7,1x10^9/l (IQR 5.6-10.3) and 224x10^9/l (IQR 169-298) respectively. In 1189 pts was assessed KS: 58% low risk, 30% intermediate risk, 12% high risk. Human erytropoetin support was given to 9% of pts. All pts received Rituximab. Planned therapeutic programs included autologous stem cells transplantation in 27% of pts, conventional chemotherapy in 67% and conventional chemotherapy plus lenalidomide in 6%. Overall 59 any grade VTE episodes occurred in 51 pts (2.9%), including 21 grade III-IV VTEs (18 pts). None was fatal. Median time from study enrollment to VTE was 63 days (IQR: 35-110). Considering death as a competitive event the 6 months cumulative incidence of VTE was 2,2% (95%IC: 1.1-3.3) in low risk, 4.5% (95%IC: 2.3-6.7) in intermediate and 6.6% (95%IC: 2.4-10.8) in high risk KS (p=0.012). KS was predictive also for grade III-IV VTEs as they were 0,7% (95%IC:0.1-1.4) in low risk and 2% (95%IC:0.8-3.3) in intermediate-high risk (p=0.048). Results were similar also after excluding lenalidomide containing studies.Fine and Gray multivariate analysis, adjusted for age and stage, showed that KS (intermediate risk adjHR=1.96; 95%IC: 0.84-4.56 and high risk adjHR=3.81; 95%IC: 1.51-9.58) and DLCL-B histotype (adjHR=2.58; 95%IC: 1.01-6.55) were independently associated to an increased risk of VTE. Moreover an ordinal logistical regression model indicated that the increase of 1 point in the KS resulted in an increased risk of VTE (OR=1.85; 95%CI: 1.23-2.79).
Conclusion
Our results suggest that DLCL-B hystotype and KS are predictors of VTE in NHL. The latter might become a simple and effective tool to assess the risk of VTE in NHL. Prospective validation including also pts not eligible for clinical trials is needed.
Session topic: E-poster
Keyword(s): Chemotherapy toxicity, Diffuse large B cell lymphoma, Thrombosis
Abstract: E951
Type: Eposter Presentation
Background
Recent studies show that the risk of VTE in Non Hodgkin Lymphoma (NHL) patients (pts) is similar to that observed in high risk solid tumors (i.e. pancreatic, ovarian cancer). VTE in NHL occurs in most cases within 3 months from diagnosis and can have substantial impact on treatment delivery and outcome as well as on quality of life. However few data are available on potential predictors.
Aims
To better clarify the epidemiology of early (within 6 months from treatment start) VTE in NHL pts we conducted a pooled data analysis of 12 clinical trials from FIL. Our analysis included basic demographic features, lymphoma-related characteristics as well as the Khorana score KS (based on histology, body mass index BMI, platelets count PLTs, white blood cells count WBC and hemoglobin values Hb) which is extensively used in solid tumors to predict VTE risk.
Methods
From Jan. 2010 to Dec. 2014 all pts with B-cell NHL enrolled in prospective clinical trials from FIL for frontline treatment were included. For 9 studies the study period included the entire trial population. The analysis was conducted based on CRFs as well as pharmacovigilance reports. VTE definition and grading was stated according to standard criteria of toxicity (CTCAE V4.0). Cumulative incidence of VTE from study enrollment was estimated using the method described by Gooley et al. accounting for death from any causes as a competing risk. The Fine & Gray survival model was used to identify predictors of VTE among NHL pts. Factors predicting the grade of VTE were investigated using an ordinal logistic regression model. This pooled data analysis was approved by local IRB.
Results
Overall, 1717 pts belonging to 12 studies were evaluated. 8 studies were phase I/II or II (25% of pts) and 4 phase III (75% of pts). M/F ratio was 1.41, median age was 57 (IQ range IQR 49-66). Histologies were: diffuse large B-cell lymphoma DLCL-B 34%, follicular lymphoma FL 41%, mantle cell lymphoma MCL 18%, other 6%. Median BMI was 25 (IQR 22-28). Median Hb, WBC and PLTs counts were 13g/dl (IQR 11.5-14.2), 7,1x10^9/l (IQR 5.6-10.3) and 224x10^9/l (IQR 169-298) respectively. In 1189 pts was assessed KS: 58% low risk, 30% intermediate risk, 12% high risk. Human erytropoetin support was given to 9% of pts. All pts received Rituximab. Planned therapeutic programs included autologous stem cells transplantation in 27% of pts, conventional chemotherapy in 67% and conventional chemotherapy plus lenalidomide in 6%. Overall 59 any grade VTE episodes occurred in 51 pts (2.9%), including 21 grade III-IV VTEs (18 pts). None was fatal. Median time from study enrollment to VTE was 63 days (IQR: 35-110). Considering death as a competitive event the 6 months cumulative incidence of VTE was 2,2% (95%IC: 1.1-3.3) in low risk, 4.5% (95%IC: 2.3-6.7) in intermediate and 6.6% (95%IC: 2.4-10.8) in high risk KS (p=0.012). KS was predictive also for grade III-IV VTEs as they were 0,7% (95%IC:0.1-1.4) in low risk and 2% (95%IC:0.8-3.3) in intermediate-high risk (p=0.048). Results were similar also after excluding lenalidomide containing studies.Fine and Gray multivariate analysis, adjusted for age and stage, showed that KS (intermediate risk adjHR=1.96; 95%IC: 0.84-4.56 and high risk adjHR=3.81; 95%IC: 1.51-9.58) and DLCL-B histotype (adjHR=2.58; 95%IC: 1.01-6.55) were independently associated to an increased risk of VTE. Moreover an ordinal logistical regression model indicated that the increase of 1 point in the KS resulted in an increased risk of VTE (OR=1.85; 95%CI: 1.23-2.79).
Conclusion
Our results suggest that DLCL-B hystotype and KS are predictors of VTE in NHL. The latter might become a simple and effective tool to assess the risk of VTE in NHL. Prospective validation including also pts not eligible for clinical trials is needed.
Session topic: E-poster
Keyword(s): Chemotherapy toxicity, Diffuse large B cell lymphoma, Thrombosis
Type: Eposter Presentation
Background
Recent studies show that the risk of VTE in Non Hodgkin Lymphoma (NHL) patients (pts) is similar to that observed in high risk solid tumors (i.e. pancreatic, ovarian cancer). VTE in NHL occurs in most cases within 3 months from diagnosis and can have substantial impact on treatment delivery and outcome as well as on quality of life. However few data are available on potential predictors.
Aims
To better clarify the epidemiology of early (within 6 months from treatment start) VTE in NHL pts we conducted a pooled data analysis of 12 clinical trials from FIL. Our analysis included basic demographic features, lymphoma-related characteristics as well as the Khorana score KS (based on histology, body mass index BMI, platelets count PLTs, white blood cells count WBC and hemoglobin values Hb) which is extensively used in solid tumors to predict VTE risk.
Methods
From Jan. 2010 to Dec. 2014 all pts with B-cell NHL enrolled in prospective clinical trials from FIL for frontline treatment were included. For 9 studies the study period included the entire trial population. The analysis was conducted based on CRFs as well as pharmacovigilance reports. VTE definition and grading was stated according to standard criteria of toxicity (CTCAE V4.0). Cumulative incidence of VTE from study enrollment was estimated using the method described by Gooley et al. accounting for death from any causes as a competing risk. The Fine & Gray survival model was used to identify predictors of VTE among NHL pts. Factors predicting the grade of VTE were investigated using an ordinal logistic regression model. This pooled data analysis was approved by local IRB.
Results
Overall, 1717 pts belonging to 12 studies were evaluated. 8 studies were phase I/II or II (25% of pts) and 4 phase III (75% of pts). M/F ratio was 1.41, median age was 57 (IQ range IQR 49-66). Histologies were: diffuse large B-cell lymphoma DLCL-B 34%, follicular lymphoma FL 41%, mantle cell lymphoma MCL 18%, other 6%. Median BMI was 25 (IQR 22-28). Median Hb, WBC and PLTs counts were 13g/dl (IQR 11.5-14.2), 7,1x10^9/l (IQR 5.6-10.3) and 224x10^9/l (IQR 169-298) respectively. In 1189 pts was assessed KS: 58% low risk, 30% intermediate risk, 12% high risk. Human erytropoetin support was given to 9% of pts. All pts received Rituximab. Planned therapeutic programs included autologous stem cells transplantation in 27% of pts, conventional chemotherapy in 67% and conventional chemotherapy plus lenalidomide in 6%. Overall 59 any grade VTE episodes occurred in 51 pts (2.9%), including 21 grade III-IV VTEs (18 pts). None was fatal. Median time from study enrollment to VTE was 63 days (IQR: 35-110). Considering death as a competitive event the 6 months cumulative incidence of VTE was 2,2% (95%IC: 1.1-3.3) in low risk, 4.5% (95%IC: 2.3-6.7) in intermediate and 6.6% (95%IC: 2.4-10.8) in high risk KS (p=0.012). KS was predictive also for grade III-IV VTEs as they were 0,7% (95%IC:0.1-1.4) in low risk and 2% (95%IC:0.8-3.3) in intermediate-high risk (p=0.048). Results were similar also after excluding lenalidomide containing studies.Fine and Gray multivariate analysis, adjusted for age and stage, showed that KS (intermediate risk adjHR=1.96; 95%IC: 0.84-4.56 and high risk adjHR=3.81; 95%IC: 1.51-9.58) and DLCL-B histotype (adjHR=2.58; 95%IC: 1.01-6.55) were independently associated to an increased risk of VTE. Moreover an ordinal logistical regression model indicated that the increase of 1 point in the KS resulted in an increased risk of VTE (OR=1.85; 95%CI: 1.23-2.79).
Conclusion
Our results suggest that DLCL-B hystotype and KS are predictors of VTE in NHL. The latter might become a simple and effective tool to assess the risk of VTE in NHL. Prospective validation including also pts not eligible for clinical trials is needed.
Session topic: E-poster
Keyword(s): Chemotherapy toxicity, Diffuse large B cell lymphoma, Thrombosis
{{ help_message }}
{{filter}}


