VALIDATION OF NCCN INTERNATIONAL PROGNOSTIC INDEX (NCCN-IPI) FOR DIFFUSE LARGE B-CELL LYMPHOMA (DLBCL). THE ADDITION OF Β2MICROGLOBULIN RESULTED IN GELTAMO-IPI THAT IS MORE ACCURATE.
(Abstract release date: 05/19/16)
EHA Library. Montalban C. 06/09/16; 132495; E946

Dr. Carlos Montalban
Contributions
Contributions
Abstract
Abstract: E946
Type: Eposter Presentation
Background
The NCCN International Prognostic Index (NCCN-IPI) for patients with DLBCL treated in the rituximab era showed enhanced discrimination in the original study, when compared to IPI. However, in our previous study (ASH 2015 #3955) it failed to identify patients with a real poor outcome.
Aims
In the present study we explore the prognostic effect of adding new factors to the variables of NCCN-IPI in a large series of patients.
Methods
This nation-wide retrospective study includes a final database of 1848 patients with de novo DLBCL diagnosed in 20 Spanish centers within the Grupo Español de Linfomas/ Transplante de Médula Osea (GELTAMO) network treated with standard chemotherapy and rituximab. To study the improvement of the prognostic effect of adding three new variables, normalized high serum β2 microglobulin (β2mcg), primary extranodal involvement and treatments more intense than R-CHOP, to the NCCN-IPI variables, the series was split in two cohorts. The training cohort (1230 patients) was used to develop a prognostic model using Cox regression models for Overall Survival and the final model was validated in an independent validation cohort (618 patients). The Kaplan Meyer method and log-rank test were used for OS and comparison of curves. The prognostic effect of this score was compared with NCCN-IPI and IPI with the reclassification calibration statistics (a modification of Hosmer–Lemeshow goodness of fit).
Results
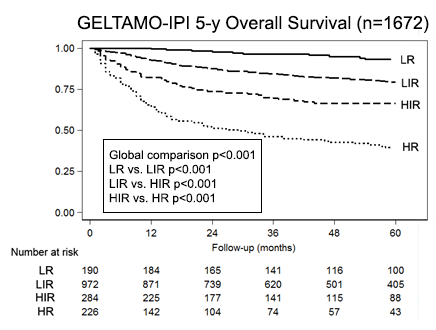
The COX regression model in the training cohort, showed that distinct extranodal involvement (as included in NCCN-IPI), primary extranodal lymphoma and intense treatment achieved no significance. The final model included the rest of the variables, with points according with the hazard ratios: age (<65/0 pts; ≥65-79/1 pt; ≥80/2 pts), PS(0-1/0 pts ; 2/1 pt ;≥2/2 pts), high LDH, Stage III-IV and high β2mcg, with 1 point each, resulting in a score (GELTAMO-IPI) with a maximum of 7 points that separated significantly four risk groups: LR (0 points), LIR (1-3 pts), HIR (4 pts), HR (≥5) with significantly different 5-yOS that was subsequently confirmed in the validation cohort. Using all the patients in the series with available data (n=1672), GELTAMO-IPI discriminates better (5-yOS rates of LR: 93%, LIR 79%, HIR 66%, HR 39%) than NCCN-IPI (93%, 83%, 67%, 49%, respectively) and IPI (88%, 77%, 68%, 51%, respectively); both NCCN-IPI and IPI failed to identify a population with a 5-yOS substantially lower that 50%. Similar results were obtained for 5-yFFS. In the reclassification calibration statistics GELTAMO-IPI was more accurate than NCCN-IPI and IPI.
Conclusion
GELTAMO-IPI including β2mcg along all the variables of NCCN-IPI (excluding selective extranodal involvement) is more accurate than NCCN-IPI and IPI for the prognosis of DLBCL. Additionally, it can be used in primary nodal and extranodal lymphoma and in patients with intense treatment and, most important, identifies a poor prognostic group with 5y-OS of 39%.
Session topic: E-poster
Keyword(s): DLBCL, Prognosis, Prognostic groups, Risk factor
Type: Eposter Presentation
Background
The NCCN International Prognostic Index (NCCN-IPI) for patients with DLBCL treated in the rituximab era showed enhanced discrimination in the original study, when compared to IPI. However, in our previous study (ASH 2015 #3955) it failed to identify patients with a real poor outcome.
Aims
In the present study we explore the prognostic effect of adding new factors to the variables of NCCN-IPI in a large series of patients.
Methods
This nation-wide retrospective study includes a final database of 1848 patients with de novo DLBCL diagnosed in 20 Spanish centers within the Grupo Español de Linfomas/ Transplante de Médula Osea (GELTAMO) network treated with standard chemotherapy and rituximab. To study the improvement of the prognostic effect of adding three new variables, normalized high serum β2 microglobulin (β2mcg), primary extranodal involvement and treatments more intense than R-CHOP, to the NCCN-IPI variables, the series was split in two cohorts. The training cohort (1230 patients) was used to develop a prognostic model using Cox regression models for Overall Survival and the final model was validated in an independent validation cohort (618 patients). The Kaplan Meyer method and log-rank test were used for OS and comparison of curves. The prognostic effect of this score was compared with NCCN-IPI and IPI with the reclassification calibration statistics (a modification of Hosmer–Lemeshow goodness of fit).
Results
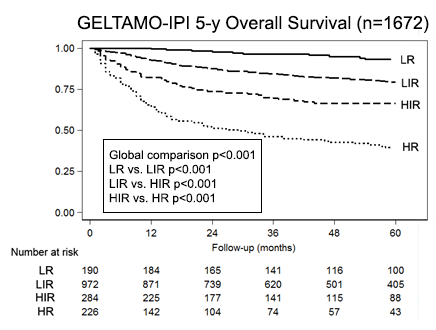
The COX regression model in the training cohort, showed that distinct extranodal involvement (as included in NCCN-IPI), primary extranodal lymphoma and intense treatment achieved no significance. The final model included the rest of the variables, with points according with the hazard ratios: age (<65/0 pts; ≥65-79/1 pt; ≥80/2 pts), PS(0-1/0 pts ; 2/1 pt ;≥2/2 pts), high LDH, Stage III-IV and high β2mcg, with 1 point each, resulting in a score (GELTAMO-IPI) with a maximum of 7 points that separated significantly four risk groups: LR (0 points), LIR (1-3 pts), HIR (4 pts), HR (≥5) with significantly different 5-yOS that was subsequently confirmed in the validation cohort. Using all the patients in the series with available data (n=1672), GELTAMO-IPI discriminates better (5-yOS rates of LR: 93%, LIR 79%, HIR 66%, HR 39%) than NCCN-IPI (93%, 83%, 67%, 49%, respectively) and IPI (88%, 77%, 68%, 51%, respectively); both NCCN-IPI and IPI failed to identify a population with a 5-yOS substantially lower that 50%. Similar results were obtained for 5-yFFS. In the reclassification calibration statistics GELTAMO-IPI was more accurate than NCCN-IPI and IPI.
Conclusion
GELTAMO-IPI including β2mcg along all the variables of NCCN-IPI (excluding selective extranodal involvement) is more accurate than NCCN-IPI and IPI for the prognosis of DLBCL. Additionally, it can be used in primary nodal and extranodal lymphoma and in patients with intense treatment and, most important, identifies a poor prognostic group with 5y-OS of 39%.
Session topic: E-poster
Keyword(s): DLBCL, Prognosis, Prognostic groups, Risk factor
Abstract: E946
Type: Eposter Presentation
Background
The NCCN International Prognostic Index (NCCN-IPI) for patients with DLBCL treated in the rituximab era showed enhanced discrimination in the original study, when compared to IPI. However, in our previous study (ASH 2015 #3955) it failed to identify patients with a real poor outcome.
Aims
In the present study we explore the prognostic effect of adding new factors to the variables of NCCN-IPI in a large series of patients.
Methods
This nation-wide retrospective study includes a final database of 1848 patients with de novo DLBCL diagnosed in 20 Spanish centers within the Grupo Español de Linfomas/ Transplante de Médula Osea (GELTAMO) network treated with standard chemotherapy and rituximab. To study the improvement of the prognostic effect of adding three new variables, normalized high serum β2 microglobulin (β2mcg), primary extranodal involvement and treatments more intense than R-CHOP, to the NCCN-IPI variables, the series was split in two cohorts. The training cohort (1230 patients) was used to develop a prognostic model using Cox regression models for Overall Survival and the final model was validated in an independent validation cohort (618 patients). The Kaplan Meyer method and log-rank test were used for OS and comparison of curves. The prognostic effect of this score was compared with NCCN-IPI and IPI with the reclassification calibration statistics (a modification of Hosmer–Lemeshow goodness of fit).
Results
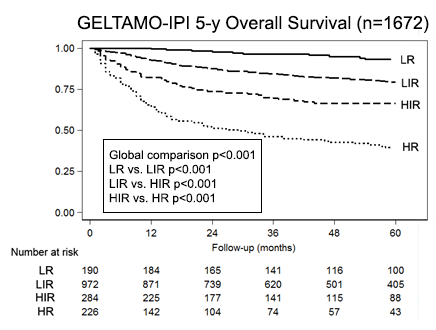
The COX regression model in the training cohort, showed that distinct extranodal involvement (as included in NCCN-IPI), primary extranodal lymphoma and intense treatment achieved no significance. The final model included the rest of the variables, with points according with the hazard ratios: age (<65/0 pts; ≥65-79/1 pt; ≥80/2 pts), PS(0-1/0 pts ; 2/1 pt ;≥2/2 pts), high LDH, Stage III-IV and high β2mcg, with 1 point each, resulting in a score (GELTAMO-IPI) with a maximum of 7 points that separated significantly four risk groups: LR (0 points), LIR (1-3 pts), HIR (4 pts), HR (≥5) with significantly different 5-yOS that was subsequently confirmed in the validation cohort. Using all the patients in the series with available data (n=1672), GELTAMO-IPI discriminates better (5-yOS rates of LR: 93%, LIR 79%, HIR 66%, HR 39%) than NCCN-IPI (93%, 83%, 67%, 49%, respectively) and IPI (88%, 77%, 68%, 51%, respectively); both NCCN-IPI and IPI failed to identify a population with a 5-yOS substantially lower that 50%. Similar results were obtained for 5-yFFS. In the reclassification calibration statistics GELTAMO-IPI was more accurate than NCCN-IPI and IPI.
Conclusion
GELTAMO-IPI including β2mcg along all the variables of NCCN-IPI (excluding selective extranodal involvement) is more accurate than NCCN-IPI and IPI for the prognosis of DLBCL. Additionally, it can be used in primary nodal and extranodal lymphoma and in patients with intense treatment and, most important, identifies a poor prognostic group with 5y-OS of 39%.
Session topic: E-poster
Keyword(s): DLBCL, Prognosis, Prognostic groups, Risk factor
Type: Eposter Presentation
Background
The NCCN International Prognostic Index (NCCN-IPI) for patients with DLBCL treated in the rituximab era showed enhanced discrimination in the original study, when compared to IPI. However, in our previous study (ASH 2015 #3955) it failed to identify patients with a real poor outcome.
Aims
In the present study we explore the prognostic effect of adding new factors to the variables of NCCN-IPI in a large series of patients.
Methods
This nation-wide retrospective study includes a final database of 1848 patients with de novo DLBCL diagnosed in 20 Spanish centers within the Grupo Español de Linfomas/ Transplante de Médula Osea (GELTAMO) network treated with standard chemotherapy and rituximab. To study the improvement of the prognostic effect of adding three new variables, normalized high serum β2 microglobulin (β2mcg), primary extranodal involvement and treatments more intense than R-CHOP, to the NCCN-IPI variables, the series was split in two cohorts. The training cohort (1230 patients) was used to develop a prognostic model using Cox regression models for Overall Survival and the final model was validated in an independent validation cohort (618 patients). The Kaplan Meyer method and log-rank test were used for OS and comparison of curves. The prognostic effect of this score was compared with NCCN-IPI and IPI with the reclassification calibration statistics (a modification of Hosmer–Lemeshow goodness of fit).
Results
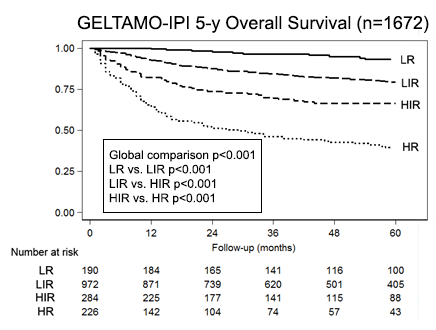
The COX regression model in the training cohort, showed that distinct extranodal involvement (as included in NCCN-IPI), primary extranodal lymphoma and intense treatment achieved no significance. The final model included the rest of the variables, with points according with the hazard ratios: age (<65/0 pts; ≥65-79/1 pt; ≥80/2 pts), PS(0-1/0 pts ; 2/1 pt ;≥2/2 pts), high LDH, Stage III-IV and high β2mcg, with 1 point each, resulting in a score (GELTAMO-IPI) with a maximum of 7 points that separated significantly four risk groups: LR (0 points), LIR (1-3 pts), HIR (4 pts), HR (≥5) with significantly different 5-yOS that was subsequently confirmed in the validation cohort. Using all the patients in the series with available data (n=1672), GELTAMO-IPI discriminates better (5-yOS rates of LR: 93%, LIR 79%, HIR 66%, HR 39%) than NCCN-IPI (93%, 83%, 67%, 49%, respectively) and IPI (88%, 77%, 68%, 51%, respectively); both NCCN-IPI and IPI failed to identify a population with a 5-yOS substantially lower that 50%. Similar results were obtained for 5-yFFS. In the reclassification calibration statistics GELTAMO-IPI was more accurate than NCCN-IPI and IPI.
Conclusion
GELTAMO-IPI including β2mcg along all the variables of NCCN-IPI (excluding selective extranodal involvement) is more accurate than NCCN-IPI and IPI for the prognosis of DLBCL. Additionally, it can be used in primary nodal and extranodal lymphoma and in patients with intense treatment and, most important, identifies a poor prognostic group with 5y-OS of 39%.
Session topic: E-poster
Keyword(s): DLBCL, Prognosis, Prognostic groups, Risk factor
{{ help_message }}
{{filter}}


