COMPARISON OF AUTOLOGOUS PERIPHERAL BLOOD STEM CELL TRANSPLANTATION TO INTENSIVE CONSOLIDATION CHEMOTHERAPY AND MONITORING MINIMAL RESIDUAL DISEASE IN CORE BINDING FACTOR ACUTE MYELOID LEUKEMIA
(Abstract release date: 05/19/16)
EHA Library. Kim H. 06/09/16; 132491; E942

Mrs. Hee Kyung Kim
Contributions
Contributions
Abstract
Abstract: E942
Type: Eposter Presentation
Background
One third of patients with core binding factor (CBF) acute myeloid leukemia (AML) relapse and disease relapse is most common cause of treatment failure. For detecting relapse, quantitative RT-PCR of AML1-ETO or CBFB-MYH11 fusion transcript is used to evaluate minimal residual disease (MRD).
Aims
The purpose of this study was to compare the clinical outcome of post-remission therapy between autologous peripheral stem cell transplantation (ASCT) and intensive consolidation chemotherapy in CBF AML patients and to assess MRD in patients who accomplished first CR(CR1) after induction chemotherapy using quantitative RT-PCR of AML1-ETO transcript.
Methods
We retrospectively analyzed adult patients who diagnosed with CBF AML between March 1996 and July 2014, and achieved CR1 after induction chemotherapy at Samsung Medical Center. The patients were divided into two groups who received ASCT or 3 to 4 cycles of intensive consolidation chemotherapy as post-remission therapy. In addition, we also investigated the impact of MRD after induction chemotherapy using quantitative RT-PCR of AML1-ETO for patient with t(8;21). AML1-ETO transripts were normalized to ABL.
Results
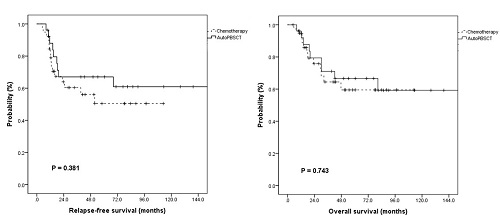
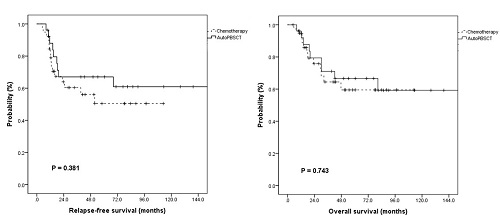
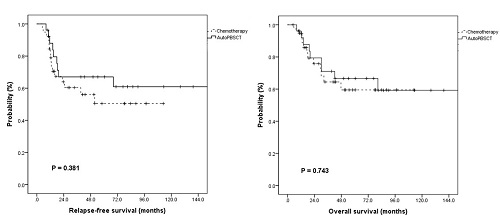
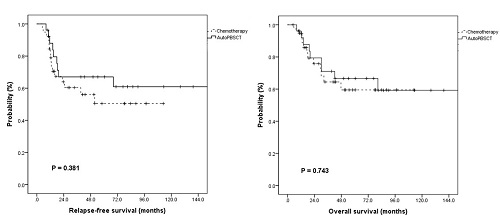
We identified 65 patients (Male=33, Female=32; t(8;21)=45, inv(16)=20) and the median age at diagnosis was 42 years(range 18-64). 26 patients (40%) received ASCT as postremission therapy and 40 patients were treated with 3 to 4 cycles of intensive chemotherapy. The ASCT group showed a better 5-year relapse free survival (RFS) rate (50.5% vs 67.0 %, p=0.381) and similar 5-year overall survival (OS) rate (59.5% vs 66.6%, p=0.743) during median follow-up 96 months. The median value of AML1-ETO mRNA levels in bone marrow was higher in relapsed patients with t(8;21) than non-relapsed patients (425.79 vs 3.29, per ABL x 103, p = 0.045). We determined cutoff for MRD as the median value of AML1-ETO transcript of all patients with t(8;21), 3.39 per ABL x 103. The 5-year RFS rates in the patients without and with MRD were 87.5% and 68.6%, respectively. (p=0.391)
Conclusion
This study demonstrated that ASCT as postremission therapy showed a better RFS than chemotherapy alone in patients with CBF AML, monitoring minimal residual disease by AML1-ETO mRNA levels as surrogate marker of patients with t(8;21) in CR1 was beneficial.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Core binding factor leukemia, Minimal residual disease (MRD)
Type: Eposter Presentation
Background
One third of patients with core binding factor (CBF) acute myeloid leukemia (AML) relapse and disease relapse is most common cause of treatment failure. For detecting relapse, quantitative RT-PCR of AML1-ETO or CBFB-MYH11 fusion transcript is used to evaluate minimal residual disease (MRD).
Aims
The purpose of this study was to compare the clinical outcome of post-remission therapy between autologous peripheral stem cell transplantation (ASCT) and intensive consolidation chemotherapy in CBF AML patients and to assess MRD in patients who accomplished first CR(CR1) after induction chemotherapy using quantitative RT-PCR of AML1-ETO transcript.
Methods
We retrospectively analyzed adult patients who diagnosed with CBF AML between March 1996 and July 2014, and achieved CR1 after induction chemotherapy at Samsung Medical Center. The patients were divided into two groups who received ASCT or 3 to 4 cycles of intensive consolidation chemotherapy as post-remission therapy. In addition, we also investigated the impact of MRD after induction chemotherapy using quantitative RT-PCR of AML1-ETO for patient with t(8;21). AML1-ETO transripts were normalized to ABL.
Results
We identified 65 patients (Male=33, Female=32; t(8;21)=45, inv(16)=20) and the median age at diagnosis was 42 years(range 18-64). 26 patients (40%) received ASCT as postremission therapy and 40 patients were treated with 3 to 4 cycles of intensive chemotherapy. The ASCT group showed a better 5-year relapse free survival (RFS) rate (50.5% vs 67.0 %, p=0.381) and similar 5-year overall survival (OS) rate (59.5% vs 66.6%, p=0.743) during median follow-up 96 months. The median value of AML1-ETO mRNA levels in bone marrow was higher in relapsed patients with t(8;21) than non-relapsed patients (425.79 vs 3.29, per ABL x 103, p = 0.045). We determined cutoff for MRD as the median value of AML1-ETO transcript of all patients with t(8;21), 3.39 per ABL x 103. The 5-year RFS rates in the patients without and with MRD were 87.5% and 68.6%, respectively. (p=0.391)
Conclusion
This study demonstrated that ASCT as postremission therapy showed a better RFS than chemotherapy alone in patients with CBF AML, monitoring minimal residual disease by AML1-ETO mRNA levels as surrogate marker of patients with t(8;21) in CR1 was beneficial.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Core binding factor leukemia, Minimal residual disease (MRD)
Abstract: E942
Type: Eposter Presentation
Background
One third of patients with core binding factor (CBF) acute myeloid leukemia (AML) relapse and disease relapse is most common cause of treatment failure. For detecting relapse, quantitative RT-PCR of AML1-ETO or CBFB-MYH11 fusion transcript is used to evaluate minimal residual disease (MRD).
Aims
The purpose of this study was to compare the clinical outcome of post-remission therapy between autologous peripheral stem cell transplantation (ASCT) and intensive consolidation chemotherapy in CBF AML patients and to assess MRD in patients who accomplished first CR(CR1) after induction chemotherapy using quantitative RT-PCR of AML1-ETO transcript.
Methods
We retrospectively analyzed adult patients who diagnosed with CBF AML between March 1996 and July 2014, and achieved CR1 after induction chemotherapy at Samsung Medical Center. The patients were divided into two groups who received ASCT or 3 to 4 cycles of intensive consolidation chemotherapy as post-remission therapy. In addition, we also investigated the impact of MRD after induction chemotherapy using quantitative RT-PCR of AML1-ETO for patient with t(8;21). AML1-ETO transripts were normalized to ABL.
Results
We identified 65 patients (Male=33, Female=32; t(8;21)=45, inv(16)=20) and the median age at diagnosis was 42 years(range 18-64). 26 patients (40%) received ASCT as postremission therapy and 40 patients were treated with 3 to 4 cycles of intensive chemotherapy. The ASCT group showed a better 5-year relapse free survival (RFS) rate (50.5% vs 67.0 %, p=0.381) and similar 5-year overall survival (OS) rate (59.5% vs 66.6%, p=0.743) during median follow-up 96 months. The median value of AML1-ETO mRNA levels in bone marrow was higher in relapsed patients with t(8;21) than non-relapsed patients (425.79 vs 3.29, per ABL x 103, p = 0.045). We determined cutoff for MRD as the median value of AML1-ETO transcript of all patients with t(8;21), 3.39 per ABL x 103. The 5-year RFS rates in the patients without and with MRD were 87.5% and 68.6%, respectively. (p=0.391)
Conclusion
This study demonstrated that ASCT as postremission therapy showed a better RFS than chemotherapy alone in patients with CBF AML, monitoring minimal residual disease by AML1-ETO mRNA levels as surrogate marker of patients with t(8;21) in CR1 was beneficial.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Core binding factor leukemia, Minimal residual disease (MRD)
Type: Eposter Presentation
Background
One third of patients with core binding factor (CBF) acute myeloid leukemia (AML) relapse and disease relapse is most common cause of treatment failure. For detecting relapse, quantitative RT-PCR of AML1-ETO or CBFB-MYH11 fusion transcript is used to evaluate minimal residual disease (MRD).
Aims
The purpose of this study was to compare the clinical outcome of post-remission therapy between autologous peripheral stem cell transplantation (ASCT) and intensive consolidation chemotherapy in CBF AML patients and to assess MRD in patients who accomplished first CR(CR1) after induction chemotherapy using quantitative RT-PCR of AML1-ETO transcript.
Methods
We retrospectively analyzed adult patients who diagnosed with CBF AML between March 1996 and July 2014, and achieved CR1 after induction chemotherapy at Samsung Medical Center. The patients were divided into two groups who received ASCT or 3 to 4 cycles of intensive consolidation chemotherapy as post-remission therapy. In addition, we also investigated the impact of MRD after induction chemotherapy using quantitative RT-PCR of AML1-ETO for patient with t(8;21). AML1-ETO transripts were normalized to ABL.
Results
We identified 65 patients (Male=33, Female=32; t(8;21)=45, inv(16)=20) and the median age at diagnosis was 42 years(range 18-64). 26 patients (40%) received ASCT as postremission therapy and 40 patients were treated with 3 to 4 cycles of intensive chemotherapy. The ASCT group showed a better 5-year relapse free survival (RFS) rate (50.5% vs 67.0 %, p=0.381) and similar 5-year overall survival (OS) rate (59.5% vs 66.6%, p=0.743) during median follow-up 96 months. The median value of AML1-ETO mRNA levels in bone marrow was higher in relapsed patients with t(8;21) than non-relapsed patients (425.79 vs 3.29, per ABL x 103, p = 0.045). We determined cutoff for MRD as the median value of AML1-ETO transcript of all patients with t(8;21), 3.39 per ABL x 103. The 5-year RFS rates in the patients without and with MRD were 87.5% and 68.6%, respectively. (p=0.391)
Conclusion
This study demonstrated that ASCT as postremission therapy showed a better RFS than chemotherapy alone in patients with CBF AML, monitoring minimal residual disease by AML1-ETO mRNA levels as surrogate marker of patients with t(8;21) in CR1 was beneficial.
Session topic: E-poster
Keyword(s): Autologous peripheral blood stem cell tansplantati, Core binding factor leukemia, Minimal residual disease (MRD)
{{ help_message }}
{{filter}}


