A BLASTIC PLASMACYTOID DENDRITIC CELL NEOPLASM-LIKE PHENOTYPE IDENTIFIES A SUBGROUP OF NPM1-MUTATED AML PATIENTS WITH WORSE PROGNOSIS
(Abstract release date: 05/19/16)
EHA Library. Minetto P. 06/09/16; 132473; E924

Dr. Paola Minetto
Contributions
Contributions
Abstract
Abstract: E924
Type: Eposter Presentation
Background
NPM1-mutated acute myeloid leukemia (NPM1-mut AML) is considered by WHO classification of myeloid neoplasms a distinct entity, representing about 30% of de novo AML in adults. Isolated NPM1 mutations display a strong positive prognostic value since they are associated with high complete response rate to induction therapies, reduced relapse risk and increased overall survival. A certain degree of clinical heterogeneity is however evident among NPM1-mut patients. The prognostic relevance of NPM1-mut AML immunophenotype (IF) is unclear. NPM1-mut blasts are usually CD34 negative, CD33 and CD13 positive. “Myeloid IF” or “monocytic IF” can be distinct by the expression of monocytic antigens as HLA-DR, CD64, CD14, CD11b.
Aims
The aim of the present study was to identify leukemia-associated immunophenotypes (LAIP) in a cohort of previously untreated NPM1-mut AML patients and to possibly disclose the prognostic role of antigens-expression patterns.
Methods
We retrospectively evaluated a cohort of 38 young, de novo NPM1-mut AML patients who have been intensively treated in our institution between 2006 and 2014.All patients were treated with a fludarabine containing induction.Multi-color immunophenotypic analysis is routinely performed in our centre by analysing erythrocyte-lysed whole BM blasts collected at diagnosis to identify relevant antigen aberration patterns and the pathological leukaemia phenotype for future minimal residual disease assessment.
Results
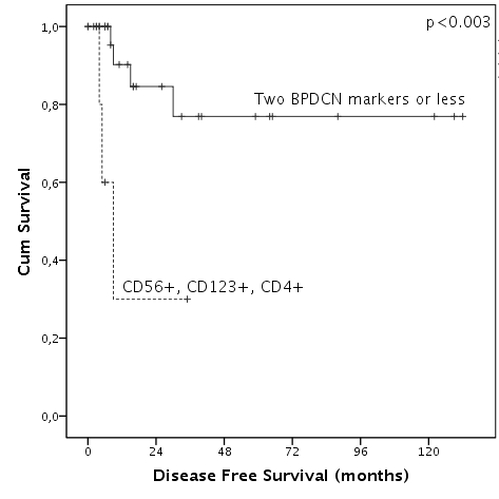
By citofluorimetric analysis three different subgroup of patients could be identified: 16/38 patients displayed a myeloid IF [CD33/CD13/CD38/CD117/MPO (+), CD16/ CD123 (-)]; 7/38 patients displayed a moncytic IF [CD33/CD64/cyLys/CD11b/CD15 (+) with 3/7 patients CD13+]; the third group included 10 patients who displayed a “myelo-monocytic IF” [CD33/CD13/CD38/CD117/MPO/CD64/cLys/CD11b/CD15 (+)]. Differently from what reported, in our experience HLA-DR displayed a heterogeneous expression and was not associated with monocytic differentiation. No statistically significant differences in relapse free survival (RFS) and overall survival (OS) were detectable among the three groups. FLT3-ITD mutation incidence was significantly higher in the monocytic group, however this did not translate in a worse outcome; as well, the expression of CD34 did not negatively affect RFS and OS.Interestingly we found that a peculiar immunophenotype CD56/CD123/CD4 (+) was recurrent in 6 patients, it was not significantly associated with one of the previously described cytofluorimetric subgroups, and was significantly associated with worse disease free survival (p <0.01, Fig. 1). Since these markers represent part of the typical immunophenotypic pattern of blastic plasmacytoid dendritic cell-neoplasm (BPDCN) we called this phenotype “BPDCN-like”. BPDCN-like phenotype was not significantly associated with the concomitant presence of FLT3-ITD mutation; moreover, median values of WT1 m-RNA expression levels were significantly lower in this subgroup of patients in comparison with the whole cohort of patients (2200 WT1/ABL copies Vs 16090 WT1/ABL, p<0.05).
Conclusion
We found a peculiar BPDCN-like immunophenotype among NPM-1 mut AML patients associated with significantly worse outcome. The biological explanation of this finding is not clear; further gene-expression profiling studies could contribute do understand our findings. We explained the lack of negative prognostic impact from FLT3-ITD mutation as consequence of the intensive fludarabine containing-induction.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Flow cytometry, Immunophenotype
Type: Eposter Presentation
Background
NPM1-mutated acute myeloid leukemia (NPM1-mut AML) is considered by WHO classification of myeloid neoplasms a distinct entity, representing about 30% of de novo AML in adults. Isolated NPM1 mutations display a strong positive prognostic value since they are associated with high complete response rate to induction therapies, reduced relapse risk and increased overall survival. A certain degree of clinical heterogeneity is however evident among NPM1-mut patients. The prognostic relevance of NPM1-mut AML immunophenotype (IF) is unclear. NPM1-mut blasts are usually CD34 negative, CD33 and CD13 positive. “Myeloid IF” or “monocytic IF” can be distinct by the expression of monocytic antigens as HLA-DR, CD64, CD14, CD11b.
Aims
The aim of the present study was to identify leukemia-associated immunophenotypes (LAIP) in a cohort of previously untreated NPM1-mut AML patients and to possibly disclose the prognostic role of antigens-expression patterns.
Methods
We retrospectively evaluated a cohort of 38 young, de novo NPM1-mut AML patients who have been intensively treated in our institution between 2006 and 2014.All patients were treated with a fludarabine containing induction.Multi-color immunophenotypic analysis is routinely performed in our centre by analysing erythrocyte-lysed whole BM blasts collected at diagnosis to identify relevant antigen aberration patterns and the pathological leukaemia phenotype for future minimal residual disease assessment.
Results
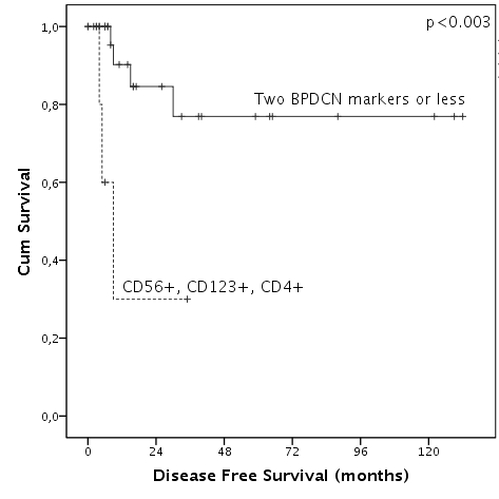
By citofluorimetric analysis three different subgroup of patients could be identified: 16/38 patients displayed a myeloid IF [CD33/CD13/CD38/CD117/MPO (+), CD16/ CD123 (-)]; 7/38 patients displayed a moncytic IF [CD33/CD64/cyLys/CD11b/CD15 (+) with 3/7 patients CD13+]; the third group included 10 patients who displayed a “myelo-monocytic IF” [CD33/CD13/CD38/CD117/MPO/CD64/cLys/CD11b/CD15 (+)]. Differently from what reported, in our experience HLA-DR displayed a heterogeneous expression and was not associated with monocytic differentiation. No statistically significant differences in relapse free survival (RFS) and overall survival (OS) were detectable among the three groups. FLT3-ITD mutation incidence was significantly higher in the monocytic group, however this did not translate in a worse outcome; as well, the expression of CD34 did not negatively affect RFS and OS.Interestingly we found that a peculiar immunophenotype CD56/CD123/CD4 (+) was recurrent in 6 patients, it was not significantly associated with one of the previously described cytofluorimetric subgroups, and was significantly associated with worse disease free survival (p <0.01, Fig. 1). Since these markers represent part of the typical immunophenotypic pattern of blastic plasmacytoid dendritic cell-neoplasm (BPDCN) we called this phenotype “BPDCN-like”. BPDCN-like phenotype was not significantly associated with the concomitant presence of FLT3-ITD mutation; moreover, median values of WT1 m-RNA expression levels were significantly lower in this subgroup of patients in comparison with the whole cohort of patients (2200 WT1/ABL copies Vs 16090 WT1/ABL, p<0.05).
Conclusion
We found a peculiar BPDCN-like immunophenotype among NPM-1 mut AML patients associated with significantly worse outcome. The biological explanation of this finding is not clear; further gene-expression profiling studies could contribute do understand our findings. We explained the lack of negative prognostic impact from FLT3-ITD mutation as consequence of the intensive fludarabine containing-induction.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Flow cytometry, Immunophenotype
Abstract: E924
Type: Eposter Presentation
Background
NPM1-mutated acute myeloid leukemia (NPM1-mut AML) is considered by WHO classification of myeloid neoplasms a distinct entity, representing about 30% of de novo AML in adults. Isolated NPM1 mutations display a strong positive prognostic value since they are associated with high complete response rate to induction therapies, reduced relapse risk and increased overall survival. A certain degree of clinical heterogeneity is however evident among NPM1-mut patients. The prognostic relevance of NPM1-mut AML immunophenotype (IF) is unclear. NPM1-mut blasts are usually CD34 negative, CD33 and CD13 positive. “Myeloid IF” or “monocytic IF” can be distinct by the expression of monocytic antigens as HLA-DR, CD64, CD14, CD11b.
Aims
The aim of the present study was to identify leukemia-associated immunophenotypes (LAIP) in a cohort of previously untreated NPM1-mut AML patients and to possibly disclose the prognostic role of antigens-expression patterns.
Methods
We retrospectively evaluated a cohort of 38 young, de novo NPM1-mut AML patients who have been intensively treated in our institution between 2006 and 2014.All patients were treated with a fludarabine containing induction.Multi-color immunophenotypic analysis is routinely performed in our centre by analysing erythrocyte-lysed whole BM blasts collected at diagnosis to identify relevant antigen aberration patterns and the pathological leukaemia phenotype for future minimal residual disease assessment.
Results
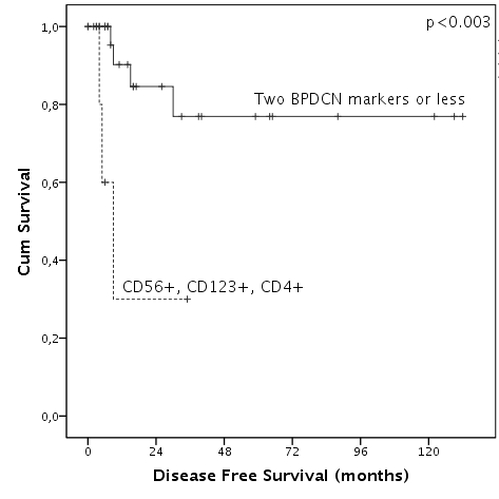
By citofluorimetric analysis three different subgroup of patients could be identified: 16/38 patients displayed a myeloid IF [CD33/CD13/CD38/CD117/MPO (+), CD16/ CD123 (-)]; 7/38 patients displayed a moncytic IF [CD33/CD64/cyLys/CD11b/CD15 (+) with 3/7 patients CD13+]; the third group included 10 patients who displayed a “myelo-monocytic IF” [CD33/CD13/CD38/CD117/MPO/CD64/cLys/CD11b/CD15 (+)]. Differently from what reported, in our experience HLA-DR displayed a heterogeneous expression and was not associated with monocytic differentiation. No statistically significant differences in relapse free survival (RFS) and overall survival (OS) were detectable among the three groups. FLT3-ITD mutation incidence was significantly higher in the monocytic group, however this did not translate in a worse outcome; as well, the expression of CD34 did not negatively affect RFS and OS.Interestingly we found that a peculiar immunophenotype CD56/CD123/CD4 (+) was recurrent in 6 patients, it was not significantly associated with one of the previously described cytofluorimetric subgroups, and was significantly associated with worse disease free survival (p <0.01, Fig. 1). Since these markers represent part of the typical immunophenotypic pattern of blastic plasmacytoid dendritic cell-neoplasm (BPDCN) we called this phenotype “BPDCN-like”. BPDCN-like phenotype was not significantly associated with the concomitant presence of FLT3-ITD mutation; moreover, median values of WT1 m-RNA expression levels were significantly lower in this subgroup of patients in comparison with the whole cohort of patients (2200 WT1/ABL copies Vs 16090 WT1/ABL, p<0.05).
Conclusion
We found a peculiar BPDCN-like immunophenotype among NPM-1 mut AML patients associated with significantly worse outcome. The biological explanation of this finding is not clear; further gene-expression profiling studies could contribute do understand our findings. We explained the lack of negative prognostic impact from FLT3-ITD mutation as consequence of the intensive fludarabine containing-induction.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Flow cytometry, Immunophenotype
Type: Eposter Presentation
Background
NPM1-mutated acute myeloid leukemia (NPM1-mut AML) is considered by WHO classification of myeloid neoplasms a distinct entity, representing about 30% of de novo AML in adults. Isolated NPM1 mutations display a strong positive prognostic value since they are associated with high complete response rate to induction therapies, reduced relapse risk and increased overall survival. A certain degree of clinical heterogeneity is however evident among NPM1-mut patients. The prognostic relevance of NPM1-mut AML immunophenotype (IF) is unclear. NPM1-mut blasts are usually CD34 negative, CD33 and CD13 positive. “Myeloid IF” or “monocytic IF” can be distinct by the expression of monocytic antigens as HLA-DR, CD64, CD14, CD11b.
Aims
The aim of the present study was to identify leukemia-associated immunophenotypes (LAIP) in a cohort of previously untreated NPM1-mut AML patients and to possibly disclose the prognostic role of antigens-expression patterns.
Methods
We retrospectively evaluated a cohort of 38 young, de novo NPM1-mut AML patients who have been intensively treated in our institution between 2006 and 2014.All patients were treated with a fludarabine containing induction.Multi-color immunophenotypic analysis is routinely performed in our centre by analysing erythrocyte-lysed whole BM blasts collected at diagnosis to identify relevant antigen aberration patterns and the pathological leukaemia phenotype for future minimal residual disease assessment.
Results
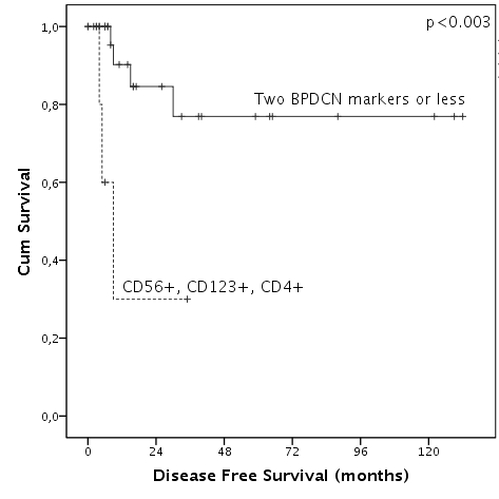
By citofluorimetric analysis three different subgroup of patients could be identified: 16/38 patients displayed a myeloid IF [CD33/CD13/CD38/CD117/MPO (+), CD16/ CD123 (-)]; 7/38 patients displayed a moncytic IF [CD33/CD64/cyLys/CD11b/CD15 (+) with 3/7 patients CD13+]; the third group included 10 patients who displayed a “myelo-monocytic IF” [CD33/CD13/CD38/CD117/MPO/CD64/cLys/CD11b/CD15 (+)]. Differently from what reported, in our experience HLA-DR displayed a heterogeneous expression and was not associated with monocytic differentiation. No statistically significant differences in relapse free survival (RFS) and overall survival (OS) were detectable among the three groups. FLT3-ITD mutation incidence was significantly higher in the monocytic group, however this did not translate in a worse outcome; as well, the expression of CD34 did not negatively affect RFS and OS.Interestingly we found that a peculiar immunophenotype CD56/CD123/CD4 (+) was recurrent in 6 patients, it was not significantly associated with one of the previously described cytofluorimetric subgroups, and was significantly associated with worse disease free survival (p <0.01, Fig. 1). Since these markers represent part of the typical immunophenotypic pattern of blastic plasmacytoid dendritic cell-neoplasm (BPDCN) we called this phenotype “BPDCN-like”. BPDCN-like phenotype was not significantly associated with the concomitant presence of FLT3-ITD mutation; moreover, median values of WT1 m-RNA expression levels were significantly lower in this subgroup of patients in comparison with the whole cohort of patients (2200 WT1/ABL copies Vs 16090 WT1/ABL, p<0.05).
Conclusion
We found a peculiar BPDCN-like immunophenotype among NPM-1 mut AML patients associated with significantly worse outcome. The biological explanation of this finding is not clear; further gene-expression profiling studies could contribute do understand our findings. We explained the lack of negative prognostic impact from FLT3-ITD mutation as consequence of the intensive fludarabine containing-induction.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Flow cytometry, Immunophenotype
{{ help_message }}
{{filter}}


