VALIDATING THE PATIENT'S 'FITNESS' CRITERIA PROPOSED TO GUIDE TREATMENT DECISION IN ELDERLY AML : A MULTICENTER STUDY ON A SERIES OF 699 PATIENTS BY THE NETWORK 'RETE EMATOLOGICA LOMBARDA'
(Abstract release date: 05/19/16)
EHA Library. Pagani C. 06/09/16; 132466; E917

Dr. Chiara Pagani
Contributions
Contributions
Abstract
Abstract: E917
Type: Eposter Presentation
Background
Treatment of elderly patients (pts) with acute myeloid leukemia (AML), is still controversial. In 2013 an Italian panel of experts proposed a set of objective criteria to define pts fit or unfit to conventional intensive chemotherapy (iCT) or non intensive therapy (niT) (Ferrara et al, Leukemia, 2013). Since such criteria derived from experts opinion, they need to be validated in the clinical setting to become an useful tool for therapy decision making.
Aims
Fitness criteria were applied to a population-based series of pts with AML (not M3), to retrospectively evaluate their actual applicability, their concordance with the treatment actually given, and the outcome of pts according to “fitness”, leukemia biology and treatment.
Methods
We evaluated 699 pts aged > 65 y, diagnosed between 2008 and 2015, at 8 Centres of the Hematological Network of Lombardy (REL). AML was de novo in 419 pts and therapy-related or secondary to myeloid neoplasms (s-AML) in 280 pts; median age was 74 (range 65-96). The categorization according to “fitness” criteria was carried out retrospectively by physicians who had followed pts and through medical files. Pts were defined as fit to iCT (FIT), unfit to iCT (UNFIT), or unfit even to niT (FRAIL). ELN prognostic criteria could be applied to 117 (27.9%) de novo AML [12.2 % favorable-risk (fav) (CBF 4.6%), 32.5% intermediate-1 (int1), 14.2% intermediate-2 (int2), and 36.4% adverse (adv) risk]. Karyotype (K) was adverse (ELN) in 193 (36%) of 537 evaluable AML. According to physicians decision, 274 pts (39.2%) received iCT, 134 pts (19.2%) niT, including low-dose ara-c, hypomethylating agents or experimental non-myelotoxic drugs, and 291 pts (41.6%) best supportive care (BSC).
Results
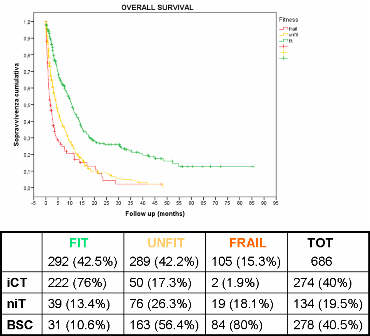
Fitness criteria were not applicable in 13 pts (1.9%), because of insufficient data. Among 686 evaluable pts, 292 (42.5%) were FIT, 289 (42.1%) UNFIT, and 105 (15.3%) FRAIL. Median age was 69, 78 and 76 y, respectively (p <0.0001). Median overall survival (OS) of FIT, UNFIT and FRAIL pts was 10.9, 4.2 and 1.8 months (m), respectively (p=0.000) (Figure 1). According to ELN risk, median OS was 17.5, 14.1, 8.0, 9.8 m, in fav, int1, int2 and adv risk de novo AML, respectively (p 0.008). Median OS was 12.6 and 5.9 m in not-adv and adv K, respectively (p 0.002).Overall concordance between “fitness criteria” and the treatment actually received by pts was 79.4% (76% in FIT, 82.7% in UNFIT and 80% in FRAIL pts). There was a significant interaction between disease biology and treatment actually given. FIT pts receiving niT had a higher proportion of adv K (66%) than pts receiving iCT (19%). In FIT pts median OS was best with iCT, being significantly longer than in pts actually “undertreated” (11.6 m with iCT vs 7.6 m with niT or BSC; p 0.006). In UNFIT pts median OS was 8.7, 9.2, 2.5 m with iCT, niT and BSC, respectively. It was significantly worse in patients actually “undertreated” with BSC only (p 0.0001), but “overtreating“ UNFIT pts with iCT did not improve OS. Among FRAIL pts, “overtreatment” using niT didn’t improve OS compared to BSC (2.9 vs 1.5 m, p:ns).
Conclusion
The “fitness criteria” proposed were easily applicable even retrospectively and in a multicenter setting. Overall concordance between “fitness criteria” and treatment actually received by pts was high (79.4%). Fitness was significantly related to patient's survival. The “fitness criteria” could correctly identify patients most likely to benefit from different treatment intensities or BSC. Knowing biologic risk profile may further refine treatment decisions.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Elderly
Type: Eposter Presentation
Background
Treatment of elderly patients (pts) with acute myeloid leukemia (AML), is still controversial. In 2013 an Italian panel of experts proposed a set of objective criteria to define pts fit or unfit to conventional intensive chemotherapy (iCT) or non intensive therapy (niT) (Ferrara et al, Leukemia, 2013). Since such criteria derived from experts opinion, they need to be validated in the clinical setting to become an useful tool for therapy decision making.
Aims
Fitness criteria were applied to a population-based series of pts with AML (not M3), to retrospectively evaluate their actual applicability, their concordance with the treatment actually given, and the outcome of pts according to “fitness”, leukemia biology and treatment.
Methods
We evaluated 699 pts aged > 65 y, diagnosed between 2008 and 2015, at 8 Centres of the Hematological Network of Lombardy (REL). AML was de novo in 419 pts and therapy-related or secondary to myeloid neoplasms (s-AML) in 280 pts; median age was 74 (range 65-96). The categorization according to “fitness” criteria was carried out retrospectively by physicians who had followed pts and through medical files. Pts were defined as fit to iCT (FIT), unfit to iCT (UNFIT), or unfit even to niT (FRAIL). ELN prognostic criteria could be applied to 117 (27.9%) de novo AML [12.2 % favorable-risk (fav) (CBF 4.6%), 32.5% intermediate-1 (int1), 14.2% intermediate-2 (int2), and 36.4% adverse (adv) risk]. Karyotype (K) was adverse (ELN) in 193 (36%) of 537 evaluable AML. According to physicians decision, 274 pts (39.2%) received iCT, 134 pts (19.2%) niT, including low-dose ara-c, hypomethylating agents or experimental non-myelotoxic drugs, and 291 pts (41.6%) best supportive care (BSC).
Results
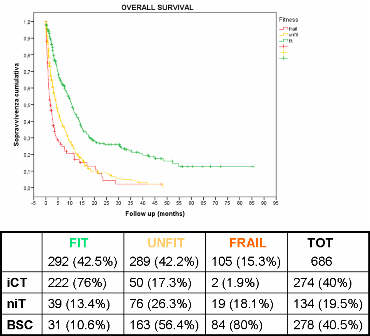
Fitness criteria were not applicable in 13 pts (1.9%), because of insufficient data. Among 686 evaluable pts, 292 (42.5%) were FIT, 289 (42.1%) UNFIT, and 105 (15.3%) FRAIL. Median age was 69, 78 and 76 y, respectively (p <0.0001). Median overall survival (OS) of FIT, UNFIT and FRAIL pts was 10.9, 4.2 and 1.8 months (m), respectively (p=0.000) (Figure 1). According to ELN risk, median OS was 17.5, 14.1, 8.0, 9.8 m, in fav, int1, int2 and adv risk de novo AML, respectively (p 0.008). Median OS was 12.6 and 5.9 m in not-adv and adv K, respectively (p 0.002).Overall concordance between “fitness criteria” and the treatment actually received by pts was 79.4% (76% in FIT, 82.7% in UNFIT and 80% in FRAIL pts). There was a significant interaction between disease biology and treatment actually given. FIT pts receiving niT had a higher proportion of adv K (66%) than pts receiving iCT (19%). In FIT pts median OS was best with iCT, being significantly longer than in pts actually “undertreated” (11.6 m with iCT vs 7.6 m with niT or BSC; p 0.006). In UNFIT pts median OS was 8.7, 9.2, 2.5 m with iCT, niT and BSC, respectively. It was significantly worse in patients actually “undertreated” with BSC only (p 0.0001), but “overtreating“ UNFIT pts with iCT did not improve OS. Among FRAIL pts, “overtreatment” using niT didn’t improve OS compared to BSC (2.9 vs 1.5 m, p:ns).
Conclusion
The “fitness criteria” proposed were easily applicable even retrospectively and in a multicenter setting. Overall concordance between “fitness criteria” and treatment actually received by pts was high (79.4%). Fitness was significantly related to patient's survival. The “fitness criteria” could correctly identify patients most likely to benefit from different treatment intensities or BSC. Knowing biologic risk profile may further refine treatment decisions.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Elderly
Abstract: E917
Type: Eposter Presentation
Background
Treatment of elderly patients (pts) with acute myeloid leukemia (AML), is still controversial. In 2013 an Italian panel of experts proposed a set of objective criteria to define pts fit or unfit to conventional intensive chemotherapy (iCT) or non intensive therapy (niT) (Ferrara et al, Leukemia, 2013). Since such criteria derived from experts opinion, they need to be validated in the clinical setting to become an useful tool for therapy decision making.
Aims
Fitness criteria were applied to a population-based series of pts with AML (not M3), to retrospectively evaluate their actual applicability, their concordance with the treatment actually given, and the outcome of pts according to “fitness”, leukemia biology and treatment.
Methods
We evaluated 699 pts aged > 65 y, diagnosed between 2008 and 2015, at 8 Centres of the Hematological Network of Lombardy (REL). AML was de novo in 419 pts and therapy-related or secondary to myeloid neoplasms (s-AML) in 280 pts; median age was 74 (range 65-96). The categorization according to “fitness” criteria was carried out retrospectively by physicians who had followed pts and through medical files. Pts were defined as fit to iCT (FIT), unfit to iCT (UNFIT), or unfit even to niT (FRAIL). ELN prognostic criteria could be applied to 117 (27.9%) de novo AML [12.2 % favorable-risk (fav) (CBF 4.6%), 32.5% intermediate-1 (int1), 14.2% intermediate-2 (int2), and 36.4% adverse (adv) risk]. Karyotype (K) was adverse (ELN) in 193 (36%) of 537 evaluable AML. According to physicians decision, 274 pts (39.2%) received iCT, 134 pts (19.2%) niT, including low-dose ara-c, hypomethylating agents or experimental non-myelotoxic drugs, and 291 pts (41.6%) best supportive care (BSC).
Results
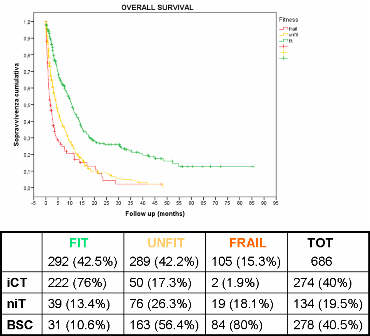
Fitness criteria were not applicable in 13 pts (1.9%), because of insufficient data. Among 686 evaluable pts, 292 (42.5%) were FIT, 289 (42.1%) UNFIT, and 105 (15.3%) FRAIL. Median age was 69, 78 and 76 y, respectively (p <0.0001). Median overall survival (OS) of FIT, UNFIT and FRAIL pts was 10.9, 4.2 and 1.8 months (m), respectively (p=0.000) (Figure 1). According to ELN risk, median OS was 17.5, 14.1, 8.0, 9.8 m, in fav, int1, int2 and adv risk de novo AML, respectively (p 0.008). Median OS was 12.6 and 5.9 m in not-adv and adv K, respectively (p 0.002).Overall concordance between “fitness criteria” and the treatment actually received by pts was 79.4% (76% in FIT, 82.7% in UNFIT and 80% in FRAIL pts). There was a significant interaction between disease biology and treatment actually given. FIT pts receiving niT had a higher proportion of adv K (66%) than pts receiving iCT (19%). In FIT pts median OS was best with iCT, being significantly longer than in pts actually “undertreated” (11.6 m with iCT vs 7.6 m with niT or BSC; p 0.006). In UNFIT pts median OS was 8.7, 9.2, 2.5 m with iCT, niT and BSC, respectively. It was significantly worse in patients actually “undertreated” with BSC only (p 0.0001), but “overtreating“ UNFIT pts with iCT did not improve OS. Among FRAIL pts, “overtreatment” using niT didn’t improve OS compared to BSC (2.9 vs 1.5 m, p:ns).
Conclusion
The “fitness criteria” proposed were easily applicable even retrospectively and in a multicenter setting. Overall concordance between “fitness criteria” and treatment actually received by pts was high (79.4%). Fitness was significantly related to patient's survival. The “fitness criteria” could correctly identify patients most likely to benefit from different treatment intensities or BSC. Knowing biologic risk profile may further refine treatment decisions.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Elderly
Type: Eposter Presentation
Background
Treatment of elderly patients (pts) with acute myeloid leukemia (AML), is still controversial. In 2013 an Italian panel of experts proposed a set of objective criteria to define pts fit or unfit to conventional intensive chemotherapy (iCT) or non intensive therapy (niT) (Ferrara et al, Leukemia, 2013). Since such criteria derived from experts opinion, they need to be validated in the clinical setting to become an useful tool for therapy decision making.
Aims
Fitness criteria were applied to a population-based series of pts with AML (not M3), to retrospectively evaluate their actual applicability, their concordance with the treatment actually given, and the outcome of pts according to “fitness”, leukemia biology and treatment.
Methods
We evaluated 699 pts aged > 65 y, diagnosed between 2008 and 2015, at 8 Centres of the Hematological Network of Lombardy (REL). AML was de novo in 419 pts and therapy-related or secondary to myeloid neoplasms (s-AML) in 280 pts; median age was 74 (range 65-96). The categorization according to “fitness” criteria was carried out retrospectively by physicians who had followed pts and through medical files. Pts were defined as fit to iCT (FIT), unfit to iCT (UNFIT), or unfit even to niT (FRAIL). ELN prognostic criteria could be applied to 117 (27.9%) de novo AML [12.2 % favorable-risk (fav) (CBF 4.6%), 32.5% intermediate-1 (int1), 14.2% intermediate-2 (int2), and 36.4% adverse (adv) risk]. Karyotype (K) was adverse (ELN) in 193 (36%) of 537 evaluable AML. According to physicians decision, 274 pts (39.2%) received iCT, 134 pts (19.2%) niT, including low-dose ara-c, hypomethylating agents or experimental non-myelotoxic drugs, and 291 pts (41.6%) best supportive care (BSC).
Results
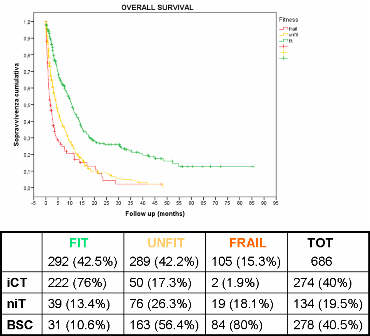
Fitness criteria were not applicable in 13 pts (1.9%), because of insufficient data. Among 686 evaluable pts, 292 (42.5%) were FIT, 289 (42.1%) UNFIT, and 105 (15.3%) FRAIL. Median age was 69, 78 and 76 y, respectively (p <0.0001). Median overall survival (OS) of FIT, UNFIT and FRAIL pts was 10.9, 4.2 and 1.8 months (m), respectively (p=0.000) (Figure 1). According to ELN risk, median OS was 17.5, 14.1, 8.0, 9.8 m, in fav, int1, int2 and adv risk de novo AML, respectively (p 0.008). Median OS was 12.6 and 5.9 m in not-adv and adv K, respectively (p 0.002).Overall concordance between “fitness criteria” and the treatment actually received by pts was 79.4% (76% in FIT, 82.7% in UNFIT and 80% in FRAIL pts). There was a significant interaction between disease biology and treatment actually given. FIT pts receiving niT had a higher proportion of adv K (66%) than pts receiving iCT (19%). In FIT pts median OS was best with iCT, being significantly longer than in pts actually “undertreated” (11.6 m with iCT vs 7.6 m with niT or BSC; p 0.006). In UNFIT pts median OS was 8.7, 9.2, 2.5 m with iCT, niT and BSC, respectively. It was significantly worse in patients actually “undertreated” with BSC only (p 0.0001), but “overtreating“ UNFIT pts with iCT did not improve OS. Among FRAIL pts, “overtreatment” using niT didn’t improve OS compared to BSC (2.9 vs 1.5 m, p:ns).
Conclusion
The “fitness criteria” proposed were easily applicable even retrospectively and in a multicenter setting. Overall concordance between “fitness criteria” and treatment actually received by pts was high (79.4%). Fitness was significantly related to patient's survival. The “fitness criteria” could correctly identify patients most likely to benefit from different treatment intensities or BSC. Knowing biologic risk profile may further refine treatment decisions.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, Elderly
{{ help_message }}
{{filter}}


