PRIMARY ACUTE MYELOID LEUKEMIA CELLS WITH OVEREXPRESSION OF EVI-1 ARE SENSITIVE TO ALL TRANS RETINOIC ACID
(Abstract release date: 05/19/16)
EHA Library. Smit L. 06/09/16; 132448; E899

Dr. Linda Smit
Contributions
Contributions
Abstract
Abstract: E899
Type: Eposter Presentation
Background
Acute Myeloid leukemia (AML) is a heterogeneous myeloid proliferative disease that can be classified based on morphology, cytogenetics, molecular aberrations, gene expression and methylation profiles. Aberrant expression of the transcriptional regulator ecotropic viral integration site-1 (EVI-1) occurs in ~10% of adult AML patients and is associated with particularly aggressive disease and a very poor outcome. Up to 95% of EVI-1 positive patients have an overall survival of less than 1 year. Therefore, there is an urgent need for novel treatment strategies to improve the survival of EVI-1 positive AML patients.For decades, most AML patients, including the group with EVI-1 overexpression, are treated with a chemotherapy combination consisting of cytarabine-arabinoside and an anthracycline. Importantly, EVI-1-positive AML patients have an very poor initial response to this currently used combination chemotherapy; 39% of EVI-1 positive patients do not achieve a complete remission after induction therapy as compared to 18% of patients in the other AML subgroups. To date, only a few alternative treatments have shown to be slightly more effective than this combination of chemotherapeutics. The exception to this is the treatment of acute promyelocytic leukemia (APL) patients with all trans retinoic acid (ATRA). ATRA treatment has significantly increased the survival chances for APL patients and has turned APL from a poor prognostic leukemia into a curable disease.
Aims
As treatment of APL patients with ATRA is very successful, we sought to determine the response to ATRA of EVI-1 positive AML patients.
Methods
Here we investigated the response of EVI-1 positive AML to ATRA (n=14) and compared this to the response of EVI-1 negative AML cases (n=7). We studied the effect of treatment with ATRA on myeloid blast differentiation, clonogenic capacity and on the in vitro and in vivo survival of AML cells.
Results
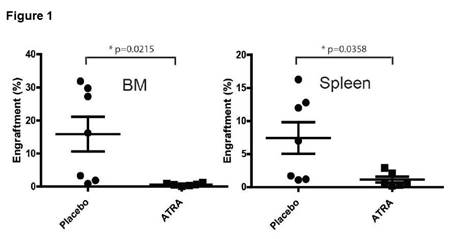
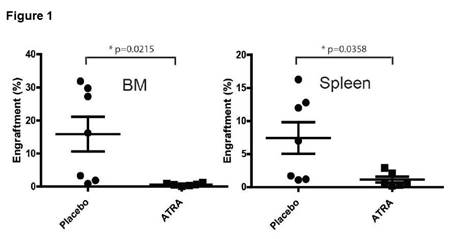
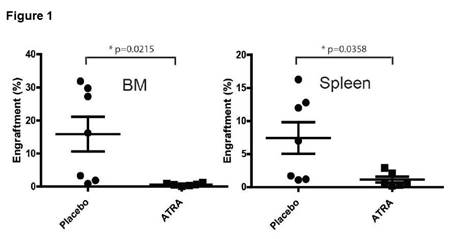
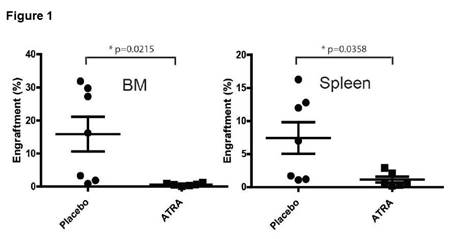
Like induction of CD11b expression on APL cells, we observed increased CD11b expression on the cell membrane of 69% of EVI-1-positive AML cases (9/13) after 7 days of incubation with ATRA. In contrast, EVI-1 negative AML cases had no induction of differentiation after ATRA treatment. In several of the EVI-1 positive AML cases, treatment with ATRA induces apoptosis of the leukemic blasts. Moreover, pre-incubation of patient EVI-1-positive AML cells with ATRA results in enhanced sensitivity to doxorubicinBesides low complete remission rates after initial treatment, the extreme poor prognosis of EVI-1-positive patients is because of high relapse rates. This relapse is due to chemotherapy resistant leukemic progenitors or leukemic stem cells (LSC). Eradication of these LSC is crucial to improve the outcome of EVI-1-positive patients. We observed a significant reduction in colony forming capacity of leukemic progenitors/stem cells in primary AML after treatment with ATRA but most importantly we demonstrated that in vivo ATRA treatment of primary EVI-1 positive AML cases leads to a significant reduction in leukemic engraftment in the bone marrow and spleen (Figure 1).
Conclusion
This study is the first to show that a considerable part of the primary EVI-1 positive AML patient samples are sensitive to ATRA treatment, suggesting that combining ATRA with conventional chemotherapy might be a promising treatment strategy for this poor prognostic subgroup of AML patients.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, ALL-trans retinoic acid (ATRA), EVI1, Therapy
Type: Eposter Presentation
Background
Acute Myeloid leukemia (AML) is a heterogeneous myeloid proliferative disease that can be classified based on morphology, cytogenetics, molecular aberrations, gene expression and methylation profiles. Aberrant expression of the transcriptional regulator ecotropic viral integration site-1 (EVI-1) occurs in ~10% of adult AML patients and is associated with particularly aggressive disease and a very poor outcome. Up to 95% of EVI-1 positive patients have an overall survival of less than 1 year. Therefore, there is an urgent need for novel treatment strategies to improve the survival of EVI-1 positive AML patients.For decades, most AML patients, including the group with EVI-1 overexpression, are treated with a chemotherapy combination consisting of cytarabine-arabinoside and an anthracycline. Importantly, EVI-1-positive AML patients have an very poor initial response to this currently used combination chemotherapy; 39% of EVI-1 positive patients do not achieve a complete remission after induction therapy as compared to 18% of patients in the other AML subgroups. To date, only a few alternative treatments have shown to be slightly more effective than this combination of chemotherapeutics. The exception to this is the treatment of acute promyelocytic leukemia (APL) patients with all trans retinoic acid (ATRA). ATRA treatment has significantly increased the survival chances for APL patients and has turned APL from a poor prognostic leukemia into a curable disease.
Aims
As treatment of APL patients with ATRA is very successful, we sought to determine the response to ATRA of EVI-1 positive AML patients.
Methods
Here we investigated the response of EVI-1 positive AML to ATRA (n=14) and compared this to the response of EVI-1 negative AML cases (n=7). We studied the effect of treatment with ATRA on myeloid blast differentiation, clonogenic capacity and on the in vitro and in vivo survival of AML cells.
Results
Like induction of CD11b expression on APL cells, we observed increased CD11b expression on the cell membrane of 69% of EVI-1-positive AML cases (9/13) after 7 days of incubation with ATRA. In contrast, EVI-1 negative AML cases had no induction of differentiation after ATRA treatment. In several of the EVI-1 positive AML cases, treatment with ATRA induces apoptosis of the leukemic blasts. Moreover, pre-incubation of patient EVI-1-positive AML cells with ATRA results in enhanced sensitivity to doxorubicinBesides low complete remission rates after initial treatment, the extreme poor prognosis of EVI-1-positive patients is because of high relapse rates. This relapse is due to chemotherapy resistant leukemic progenitors or leukemic stem cells (LSC). Eradication of these LSC is crucial to improve the outcome of EVI-1-positive patients. We observed a significant reduction in colony forming capacity of leukemic progenitors/stem cells in primary AML after treatment with ATRA but most importantly we demonstrated that in vivo ATRA treatment of primary EVI-1 positive AML cases leads to a significant reduction in leukemic engraftment in the bone marrow and spleen (Figure 1).
Conclusion
This study is the first to show that a considerable part of the primary EVI-1 positive AML patient samples are sensitive to ATRA treatment, suggesting that combining ATRA with conventional chemotherapy might be a promising treatment strategy for this poor prognostic subgroup of AML patients.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, ALL-trans retinoic acid (ATRA), EVI1, Therapy
Abstract: E899
Type: Eposter Presentation
Background
Acute Myeloid leukemia (AML) is a heterogeneous myeloid proliferative disease that can be classified based on morphology, cytogenetics, molecular aberrations, gene expression and methylation profiles. Aberrant expression of the transcriptional regulator ecotropic viral integration site-1 (EVI-1) occurs in ~10% of adult AML patients and is associated with particularly aggressive disease and a very poor outcome. Up to 95% of EVI-1 positive patients have an overall survival of less than 1 year. Therefore, there is an urgent need for novel treatment strategies to improve the survival of EVI-1 positive AML patients.For decades, most AML patients, including the group with EVI-1 overexpression, are treated with a chemotherapy combination consisting of cytarabine-arabinoside and an anthracycline. Importantly, EVI-1-positive AML patients have an very poor initial response to this currently used combination chemotherapy; 39% of EVI-1 positive patients do not achieve a complete remission after induction therapy as compared to 18% of patients in the other AML subgroups. To date, only a few alternative treatments have shown to be slightly more effective than this combination of chemotherapeutics. The exception to this is the treatment of acute promyelocytic leukemia (APL) patients with all trans retinoic acid (ATRA). ATRA treatment has significantly increased the survival chances for APL patients and has turned APL from a poor prognostic leukemia into a curable disease.
Aims
As treatment of APL patients with ATRA is very successful, we sought to determine the response to ATRA of EVI-1 positive AML patients.
Methods
Here we investigated the response of EVI-1 positive AML to ATRA (n=14) and compared this to the response of EVI-1 negative AML cases (n=7). We studied the effect of treatment with ATRA on myeloid blast differentiation, clonogenic capacity and on the in vitro and in vivo survival of AML cells.
Results
Like induction of CD11b expression on APL cells, we observed increased CD11b expression on the cell membrane of 69% of EVI-1-positive AML cases (9/13) after 7 days of incubation with ATRA. In contrast, EVI-1 negative AML cases had no induction of differentiation after ATRA treatment. In several of the EVI-1 positive AML cases, treatment with ATRA induces apoptosis of the leukemic blasts. Moreover, pre-incubation of patient EVI-1-positive AML cells with ATRA results in enhanced sensitivity to doxorubicinBesides low complete remission rates after initial treatment, the extreme poor prognosis of EVI-1-positive patients is because of high relapse rates. This relapse is due to chemotherapy resistant leukemic progenitors or leukemic stem cells (LSC). Eradication of these LSC is crucial to improve the outcome of EVI-1-positive patients. We observed a significant reduction in colony forming capacity of leukemic progenitors/stem cells in primary AML after treatment with ATRA but most importantly we demonstrated that in vivo ATRA treatment of primary EVI-1 positive AML cases leads to a significant reduction in leukemic engraftment in the bone marrow and spleen (Figure 1).
Conclusion
This study is the first to show that a considerable part of the primary EVI-1 positive AML patient samples are sensitive to ATRA treatment, suggesting that combining ATRA with conventional chemotherapy might be a promising treatment strategy for this poor prognostic subgroup of AML patients.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, ALL-trans retinoic acid (ATRA), EVI1, Therapy
Type: Eposter Presentation
Background
Acute Myeloid leukemia (AML) is a heterogeneous myeloid proliferative disease that can be classified based on morphology, cytogenetics, molecular aberrations, gene expression and methylation profiles. Aberrant expression of the transcriptional regulator ecotropic viral integration site-1 (EVI-1) occurs in ~10% of adult AML patients and is associated with particularly aggressive disease and a very poor outcome. Up to 95% of EVI-1 positive patients have an overall survival of less than 1 year. Therefore, there is an urgent need for novel treatment strategies to improve the survival of EVI-1 positive AML patients.For decades, most AML patients, including the group with EVI-1 overexpression, are treated with a chemotherapy combination consisting of cytarabine-arabinoside and an anthracycline. Importantly, EVI-1-positive AML patients have an very poor initial response to this currently used combination chemotherapy; 39% of EVI-1 positive patients do not achieve a complete remission after induction therapy as compared to 18% of patients in the other AML subgroups. To date, only a few alternative treatments have shown to be slightly more effective than this combination of chemotherapeutics. The exception to this is the treatment of acute promyelocytic leukemia (APL) patients with all trans retinoic acid (ATRA). ATRA treatment has significantly increased the survival chances for APL patients and has turned APL from a poor prognostic leukemia into a curable disease.
Aims
As treatment of APL patients with ATRA is very successful, we sought to determine the response to ATRA of EVI-1 positive AML patients.
Methods
Here we investigated the response of EVI-1 positive AML to ATRA (n=14) and compared this to the response of EVI-1 negative AML cases (n=7). We studied the effect of treatment with ATRA on myeloid blast differentiation, clonogenic capacity and on the in vitro and in vivo survival of AML cells.
Results
Like induction of CD11b expression on APL cells, we observed increased CD11b expression on the cell membrane of 69% of EVI-1-positive AML cases (9/13) after 7 days of incubation with ATRA. In contrast, EVI-1 negative AML cases had no induction of differentiation after ATRA treatment. In several of the EVI-1 positive AML cases, treatment with ATRA induces apoptosis of the leukemic blasts. Moreover, pre-incubation of patient EVI-1-positive AML cells with ATRA results in enhanced sensitivity to doxorubicinBesides low complete remission rates after initial treatment, the extreme poor prognosis of EVI-1-positive patients is because of high relapse rates. This relapse is due to chemotherapy resistant leukemic progenitors or leukemic stem cells (LSC). Eradication of these LSC is crucial to improve the outcome of EVI-1-positive patients. We observed a significant reduction in colony forming capacity of leukemic progenitors/stem cells in primary AML after treatment with ATRA but most importantly we demonstrated that in vivo ATRA treatment of primary EVI-1 positive AML cases leads to a significant reduction in leukemic engraftment in the bone marrow and spleen (Figure 1).
Conclusion
This study is the first to show that a considerable part of the primary EVI-1 positive AML patient samples are sensitive to ATRA treatment, suggesting that combining ATRA with conventional chemotherapy might be a promising treatment strategy for this poor prognostic subgroup of AML patients.
Session topic: E-poster
Keyword(s): Acute myeloid leukemia, ALL-trans retinoic acid (ATRA), EVI1, Therapy
{{ help_message }}
{{filter}}


