LONG-TERM OUTCOME OF RELAPSED ADULT PHILADELPHIA CHROMOSOME-POSITIVE ACUTE LYMPHOBLASTIC LEUKEMIA TREATED WITH CONTINUOUS IMATINIB PLUS COMBINATION CHEMOTHERAPY
(Abstract release date: 05/19/16)
EHA Library. Lim S. 06/09/16; 132422; E873

Dr. Sungnam Lim
Contributions
Contributions
Abstract
Abstract: E873
Type: Eposter Presentation
Background
Treatment outcome with conventional salvage therapy in relapsed Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) is poor and is often associated with significant morbidity. Tyrosine kinase inhibitors (TKI) have changed strategy of Ph+ ALL therapy and improved prognosis of the disease. However, despite the progress associated with TKI therapy for Ph+ ALL, the maintaining remission remains the major challenge.
Aims
We assessed the long-term outcome of relapsed adult Ph+ ALL patients treated with continuous imatinib plus combination chemotherapy.
Methods
Imatinib (600 mg/day orally) was administered continuously with combination chemotherapy, starting from eighth day of remission induction treatment, then through 5 courses of consolidation or until allogeneic hematopoietic cell transplantation (HCT). Patients who were not transplanted were maintained on imatinib for 2 years.
Results
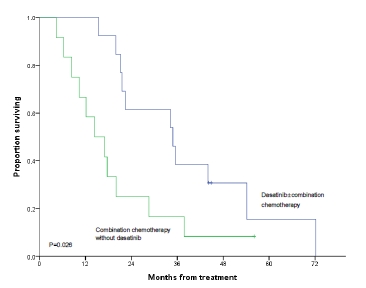
Between October 2005 and February 2009, total 87 patients, aged 16-71 years, with newly diagnosed Ph+ALL were enrolled. With median follow-up of 5 years among survivors (range: 2.6-8.9 years) and data was frozen up in May 2015. After remission induction, 82 patients (94%) achieved complete remission (CR). Among these patient, 44 patients (54%) experienced leukemia relapse and median time of leukemia relapse-free survival was 13.9 months (range, 0.4-89.5 months). Sites of relapse were bone marrow (79.5%), central nervous system (CNS) (9.1%), lymph nodes (6.8%), testis (2.3%) and pancreas (2.3%), respectively. Sixteen patients (36.4%) relapsed during consolidation treatment, 23 patients (52.3%) relapsed after allogeneic hematopoietic cell transplantation (HCT), and five patients (11.4%) relapsed during maintenance treatment after completion of five consolidation. The relapse rate within one year from CR was 45.5% in total patients and that within one year in patients underwent allogeneic HCT in first CR was 25.0%. Salvage treatments of relapsed Ph+ ALL were combination chemotherapy in 13 patients (29.5%), imatinib in 6 (13.6%), imatinib plus combination chemotherapy in 6 (13.6%), dasatinib in 8 (18.2%), dasatinib plus combination chemotherapy in 5 (11.4%), intrathecal methotrexate in 4 (9.1%) who relapsed in CNS, and to stop immunosuppressant therapy in one who underwent allogeneic HCT. One relapsed patient did not receive treatment due to poor performance state and died of leukemia recurrence. Patients treated with dasatinib±combination chemotherapy were demonstrated a longer survival compared with patients treated with combination chemotherapy without dasatinib (P=0.026). Dasatinib treatment had a tendency of superiority in survival but there was no statistical significance. Nineteen patients (43.2%) among evaluable 43 patients treated salvage therapy achieved a second CR. Two patients of them were received allogeneic HCT after achieving second CR. Eleven patients in twelve evaluable patients who achieved a second CR experienced a second relapse. The median time of survival was 21.3 months (range, 4.4-72.2 months). The causes of death of them were leukemia recurrence (89.2%), and infection (10.8%).
Conclusion
Inclusion of dasatinib into transplantation strategy allows obtaining sustained remission even in patients relapsed after imatinib treatment.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Imatinib, Relapsed acute lymphoblastic leukemia
Type: Eposter Presentation
Background
Treatment outcome with conventional salvage therapy in relapsed Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) is poor and is often associated with significant morbidity. Tyrosine kinase inhibitors (TKI) have changed strategy of Ph+ ALL therapy and improved prognosis of the disease. However, despite the progress associated with TKI therapy for Ph+ ALL, the maintaining remission remains the major challenge.
Aims
We assessed the long-term outcome of relapsed adult Ph+ ALL patients treated with continuous imatinib plus combination chemotherapy.
Methods
Imatinib (600 mg/day orally) was administered continuously with combination chemotherapy, starting from eighth day of remission induction treatment, then through 5 courses of consolidation or until allogeneic hematopoietic cell transplantation (HCT). Patients who were not transplanted were maintained on imatinib for 2 years.
Results
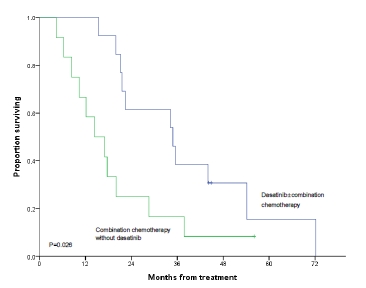
Between October 2005 and February 2009, total 87 patients, aged 16-71 years, with newly diagnosed Ph+ALL were enrolled. With median follow-up of 5 years among survivors (range: 2.6-8.9 years) and data was frozen up in May 2015. After remission induction, 82 patients (94%) achieved complete remission (CR). Among these patient, 44 patients (54%) experienced leukemia relapse and median time of leukemia relapse-free survival was 13.9 months (range, 0.4-89.5 months). Sites of relapse were bone marrow (79.5%), central nervous system (CNS) (9.1%), lymph nodes (6.8%), testis (2.3%) and pancreas (2.3%), respectively. Sixteen patients (36.4%) relapsed during consolidation treatment, 23 patients (52.3%) relapsed after allogeneic hematopoietic cell transplantation (HCT), and five patients (11.4%) relapsed during maintenance treatment after completion of five consolidation. The relapse rate within one year from CR was 45.5% in total patients and that within one year in patients underwent allogeneic HCT in first CR was 25.0%. Salvage treatments of relapsed Ph+ ALL were combination chemotherapy in 13 patients (29.5%), imatinib in 6 (13.6%), imatinib plus combination chemotherapy in 6 (13.6%), dasatinib in 8 (18.2%), dasatinib plus combination chemotherapy in 5 (11.4%), intrathecal methotrexate in 4 (9.1%) who relapsed in CNS, and to stop immunosuppressant therapy in one who underwent allogeneic HCT. One relapsed patient did not receive treatment due to poor performance state and died of leukemia recurrence. Patients treated with dasatinib±combination chemotherapy were demonstrated a longer survival compared with patients treated with combination chemotherapy without dasatinib (P=0.026). Dasatinib treatment had a tendency of superiority in survival but there was no statistical significance. Nineteen patients (43.2%) among evaluable 43 patients treated salvage therapy achieved a second CR. Two patients of them were received allogeneic HCT after achieving second CR. Eleven patients in twelve evaluable patients who achieved a second CR experienced a second relapse. The median time of survival was 21.3 months (range, 4.4-72.2 months). The causes of death of them were leukemia recurrence (89.2%), and infection (10.8%).
Conclusion
Inclusion of dasatinib into transplantation strategy allows obtaining sustained remission even in patients relapsed after imatinib treatment.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Imatinib, Relapsed acute lymphoblastic leukemia
Abstract: E873
Type: Eposter Presentation
Background
Treatment outcome with conventional salvage therapy in relapsed Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) is poor and is often associated with significant morbidity. Tyrosine kinase inhibitors (TKI) have changed strategy of Ph+ ALL therapy and improved prognosis of the disease. However, despite the progress associated with TKI therapy for Ph+ ALL, the maintaining remission remains the major challenge.
Aims
We assessed the long-term outcome of relapsed adult Ph+ ALL patients treated with continuous imatinib plus combination chemotherapy.
Methods
Imatinib (600 mg/day orally) was administered continuously with combination chemotherapy, starting from eighth day of remission induction treatment, then through 5 courses of consolidation or until allogeneic hematopoietic cell transplantation (HCT). Patients who were not transplanted were maintained on imatinib for 2 years.
Results
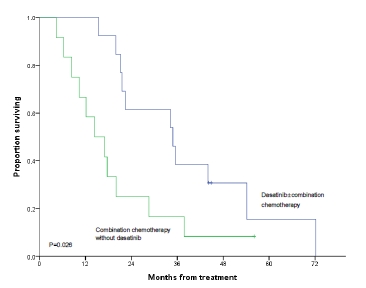
Between October 2005 and February 2009, total 87 patients, aged 16-71 years, with newly diagnosed Ph+ALL were enrolled. With median follow-up of 5 years among survivors (range: 2.6-8.9 years) and data was frozen up in May 2015. After remission induction, 82 patients (94%) achieved complete remission (CR). Among these patient, 44 patients (54%) experienced leukemia relapse and median time of leukemia relapse-free survival was 13.9 months (range, 0.4-89.5 months). Sites of relapse were bone marrow (79.5%), central nervous system (CNS) (9.1%), lymph nodes (6.8%), testis (2.3%) and pancreas (2.3%), respectively. Sixteen patients (36.4%) relapsed during consolidation treatment, 23 patients (52.3%) relapsed after allogeneic hematopoietic cell transplantation (HCT), and five patients (11.4%) relapsed during maintenance treatment after completion of five consolidation. The relapse rate within one year from CR was 45.5% in total patients and that within one year in patients underwent allogeneic HCT in first CR was 25.0%. Salvage treatments of relapsed Ph+ ALL were combination chemotherapy in 13 patients (29.5%), imatinib in 6 (13.6%), imatinib plus combination chemotherapy in 6 (13.6%), dasatinib in 8 (18.2%), dasatinib plus combination chemotherapy in 5 (11.4%), intrathecal methotrexate in 4 (9.1%) who relapsed in CNS, and to stop immunosuppressant therapy in one who underwent allogeneic HCT. One relapsed patient did not receive treatment due to poor performance state and died of leukemia recurrence. Patients treated with dasatinib±combination chemotherapy were demonstrated a longer survival compared with patients treated with combination chemotherapy without dasatinib (P=0.026). Dasatinib treatment had a tendency of superiority in survival but there was no statistical significance. Nineteen patients (43.2%) among evaluable 43 patients treated salvage therapy achieved a second CR. Two patients of them were received allogeneic HCT after achieving second CR. Eleven patients in twelve evaluable patients who achieved a second CR experienced a second relapse. The median time of survival was 21.3 months (range, 4.4-72.2 months). The causes of death of them were leukemia recurrence (89.2%), and infection (10.8%).
Conclusion
Inclusion of dasatinib into transplantation strategy allows obtaining sustained remission even in patients relapsed after imatinib treatment.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Imatinib, Relapsed acute lymphoblastic leukemia
Type: Eposter Presentation
Background
Treatment outcome with conventional salvage therapy in relapsed Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) is poor and is often associated with significant morbidity. Tyrosine kinase inhibitors (TKI) have changed strategy of Ph+ ALL therapy and improved prognosis of the disease. However, despite the progress associated with TKI therapy for Ph+ ALL, the maintaining remission remains the major challenge.
Aims
We assessed the long-term outcome of relapsed adult Ph+ ALL patients treated with continuous imatinib plus combination chemotherapy.
Methods
Imatinib (600 mg/day orally) was administered continuously with combination chemotherapy, starting from eighth day of remission induction treatment, then through 5 courses of consolidation or until allogeneic hematopoietic cell transplantation (HCT). Patients who were not transplanted were maintained on imatinib for 2 years.
Results
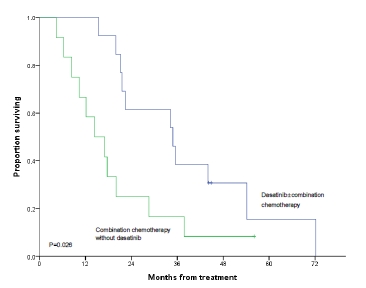
Between October 2005 and February 2009, total 87 patients, aged 16-71 years, with newly diagnosed Ph+ALL were enrolled. With median follow-up of 5 years among survivors (range: 2.6-8.9 years) and data was frozen up in May 2015. After remission induction, 82 patients (94%) achieved complete remission (CR). Among these patient, 44 patients (54%) experienced leukemia relapse and median time of leukemia relapse-free survival was 13.9 months (range, 0.4-89.5 months). Sites of relapse were bone marrow (79.5%), central nervous system (CNS) (9.1%), lymph nodes (6.8%), testis (2.3%) and pancreas (2.3%), respectively. Sixteen patients (36.4%) relapsed during consolidation treatment, 23 patients (52.3%) relapsed after allogeneic hematopoietic cell transplantation (HCT), and five patients (11.4%) relapsed during maintenance treatment after completion of five consolidation. The relapse rate within one year from CR was 45.5% in total patients and that within one year in patients underwent allogeneic HCT in first CR was 25.0%. Salvage treatments of relapsed Ph+ ALL were combination chemotherapy in 13 patients (29.5%), imatinib in 6 (13.6%), imatinib plus combination chemotherapy in 6 (13.6%), dasatinib in 8 (18.2%), dasatinib plus combination chemotherapy in 5 (11.4%), intrathecal methotrexate in 4 (9.1%) who relapsed in CNS, and to stop immunosuppressant therapy in one who underwent allogeneic HCT. One relapsed patient did not receive treatment due to poor performance state and died of leukemia recurrence. Patients treated with dasatinib±combination chemotherapy were demonstrated a longer survival compared with patients treated with combination chemotherapy without dasatinib (P=0.026). Dasatinib treatment had a tendency of superiority in survival but there was no statistical significance. Nineteen patients (43.2%) among evaluable 43 patients treated salvage therapy achieved a second CR. Two patients of them were received allogeneic HCT after achieving second CR. Eleven patients in twelve evaluable patients who achieved a second CR experienced a second relapse. The median time of survival was 21.3 months (range, 4.4-72.2 months). The causes of death of them were leukemia recurrence (89.2%), and infection (10.8%).
Conclusion
Inclusion of dasatinib into transplantation strategy allows obtaining sustained remission even in patients relapsed after imatinib treatment.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Imatinib, Relapsed acute lymphoblastic leukemia
{{ help_message }}
{{filter}}


