BFM REGIMEN OFFERS SIMILAR EVENT FREE SURVIVAL COMPARED TO HYPERCVAD BUT WITH LESS TOXICITY IN ADOLESCENTS AND YOUNG PATIENTS WITH ACUTE LYMPHOBLASTIC LEUKEMIA
(Abstract release date: 05/19/16)
EHA Library. Vega A. 06/09/16; 132413; E864

Dr. Arturo Vega
Contributions
Contributions
Abstract
Abstract: E864
Type: Eposter Presentation
Background
The experience to adapt pediatric protocols to adolescents and young adults (AYA) with acute lymphoblastic leukemia (ALL) is improving. Although there is still concern that toxicity may occur.
Aims
We present two groups of AYA treated with an adult protocol (hypercvad) and BFM developed for children. The study aimed to compare event free survival (EFS) and toxicity in both regimens.
Methods
Patients aged ≥16 and ≤40 between 2008-2015. BFM consisted of 8 blocks. Induction with vcr, pdn, asp, daunorubicine (dau) and intrathecal therapy (IT). Consolidation with ciclophosphamide (cfm), mercaptopurine (mp), cytarabine (cyt), vcr, asp and IT. CNS prophylaxis with methotrexate (mtx), followed by interim maintenance (im) combining vcr, mtx and asp. The other 4 blocks composed by delayed intensification (di) x 2 with vcr, dau, pdn, asp, cfm, mp, cyt, vcr and one im and di (as in induction). Hypercvad was prescribed with the addition of IT to each one of the 8 arms. Maintenance consisted of POMP for 2 years, and in some, combined with etoposide or anthracycline plus IT for 6 months. Rituximab (mab) was allowed at discretion if CD 20+. Ph+ cases received imatinib. Radiotherapy was permitted for mediastinal tumor. Patients changed the initial regimen if non hematological toxicity occurred during induction or by preference and registered in the regimen they continued. Variables analyzed: age (±30), WBC (≥30000 B and ≥100000 T), cytogenetic (t9;22 [ph+] and complex karyotypes), lineage, CD20, and aberrant markers. Relapse and death in CR due to toxicity were censored for the EFS analysis. Toxicity counted as one event in each block/arm (only ≥3 grade) or if admission or transfusion needed. Death during induction was excluded from the toxicity analysis.
Results
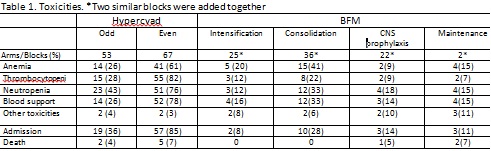
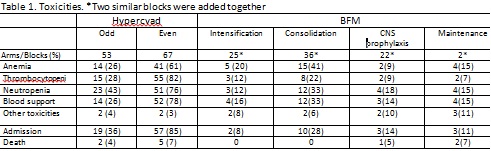
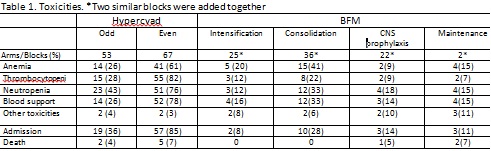
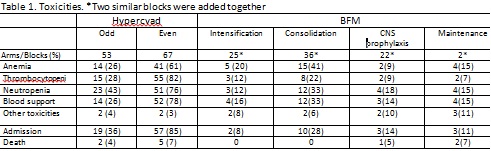
Fifty eight cases were treated. Median was 24 years (16-40). WBC was 15400 (0.6-632000). Twelve patients had karyotype and five were high risk (four ph+). Sixteen cases (33%) classified as high risk. Three cases had CNS disease. Fifty one (88%) cases were B and 48% CD 20+ (ten received mab). Seventeen had aberrant markers. Mediastinal tumor was observed in four T cell cases. The EFS of the whole group at 3 years was 30%. Forty five (78%) patients received induction with BFM with 8 deaths (17.7%), and thirteen (22%) with hypercvad with 2 deaths (15.3%). Median follow up was 12 months (1-72) with twenty one individuals in CR. Fourteen (29%) patients changed treatment, thirteen in the BFM group, 4 for pancreatitis and 9 by preference and one due to toxicity in the hypercvad group. Thirty three patients were included in BFM and twenty five in hypercvad. The EFS at three years was 32% for BFM and 28% for hypercvad p=.6. There were seventeen relapses (BFM 8 hypercvad 9) and ten deaths in CR due to toxicity (BFM 3 hypercvad 7). Toxic deaths in BFM were infectious in one and CNS toxicity in two. All toxic deaths in hypercvad were infectious Table 1. None of the variables had statistical difference. More toxic deaths occurred during the even courses and nearly 80% required admission for neutropenia and blood support (compared to a close 30% of the odd courses) in the hypercvad protocol. For the BFM, most admissions happened during consolidation (28%). The other blocks had less toxicity, although neurotoxicity occurred during maintenance. Mucositis presented barely in both groups. Coagulopathy and hepatitis rarely appeared with asp.
Conclusion
Both regimens had similar EFS but hypercvad had more deaths in CR due to myelotoxicity and more blood support and admission to the hospital. Severe non-myelotoxic events were uncommon.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Toxicity
Type: Eposter Presentation
Background
The experience to adapt pediatric protocols to adolescents and young adults (AYA) with acute lymphoblastic leukemia (ALL) is improving. Although there is still concern that toxicity may occur.
Aims
We present two groups of AYA treated with an adult protocol (hypercvad) and BFM developed for children. The study aimed to compare event free survival (EFS) and toxicity in both regimens.
Methods
Patients aged ≥16 and ≤40 between 2008-2015. BFM consisted of 8 blocks. Induction with vcr, pdn, asp, daunorubicine (dau) and intrathecal therapy (IT). Consolidation with ciclophosphamide (cfm), mercaptopurine (mp), cytarabine (cyt), vcr, asp and IT. CNS prophylaxis with methotrexate (mtx), followed by interim maintenance (im) combining vcr, mtx and asp. The other 4 blocks composed by delayed intensification (di) x 2 with vcr, dau, pdn, asp, cfm, mp, cyt, vcr and one im and di (as in induction). Hypercvad was prescribed with the addition of IT to each one of the 8 arms. Maintenance consisted of POMP for 2 years, and in some, combined with etoposide or anthracycline plus IT for 6 months. Rituximab (mab) was allowed at discretion if CD 20+. Ph+ cases received imatinib. Radiotherapy was permitted for mediastinal tumor. Patients changed the initial regimen if non hematological toxicity occurred during induction or by preference and registered in the regimen they continued. Variables analyzed: age (±30), WBC (≥30000 B and ≥100000 T), cytogenetic (t9;22 [ph+] and complex karyotypes), lineage, CD20, and aberrant markers. Relapse and death in CR due to toxicity were censored for the EFS analysis. Toxicity counted as one event in each block/arm (only ≥3 grade) or if admission or transfusion needed. Death during induction was excluded from the toxicity analysis.
Results
Fifty eight cases were treated. Median was 24 years (16-40). WBC was 15400 (0.6-632000). Twelve patients had karyotype and five were high risk (four ph+). Sixteen cases (33%) classified as high risk. Three cases had CNS disease. Fifty one (88%) cases were B and 48% CD 20+ (ten received mab). Seventeen had aberrant markers. Mediastinal tumor was observed in four T cell cases. The EFS of the whole group at 3 years was 30%. Forty five (78%) patients received induction with BFM with 8 deaths (17.7%), and thirteen (22%) with hypercvad with 2 deaths (15.3%). Median follow up was 12 months (1-72) with twenty one individuals in CR. Fourteen (29%) patients changed treatment, thirteen in the BFM group, 4 for pancreatitis and 9 by preference and one due to toxicity in the hypercvad group. Thirty three patients were included in BFM and twenty five in hypercvad. The EFS at three years was 32% for BFM and 28% for hypercvad p=.6. There were seventeen relapses (BFM 8 hypercvad 9) and ten deaths in CR due to toxicity (BFM 3 hypercvad 7). Toxic deaths in BFM were infectious in one and CNS toxicity in two. All toxic deaths in hypercvad were infectious Table 1. None of the variables had statistical difference. More toxic deaths occurred during the even courses and nearly 80% required admission for neutropenia and blood support (compared to a close 30% of the odd courses) in the hypercvad protocol. For the BFM, most admissions happened during consolidation (28%). The other blocks had less toxicity, although neurotoxicity occurred during maintenance. Mucositis presented barely in both groups. Coagulopathy and hepatitis rarely appeared with asp.
Conclusion
Both regimens had similar EFS but hypercvad had more deaths in CR due to myelotoxicity and more blood support and admission to the hospital. Severe non-myelotoxic events were uncommon.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Toxicity
Abstract: E864
Type: Eposter Presentation
Background
The experience to adapt pediatric protocols to adolescents and young adults (AYA) with acute lymphoblastic leukemia (ALL) is improving. Although there is still concern that toxicity may occur.
Aims
We present two groups of AYA treated with an adult protocol (hypercvad) and BFM developed for children. The study aimed to compare event free survival (EFS) and toxicity in both regimens.
Methods
Patients aged ≥16 and ≤40 between 2008-2015. BFM consisted of 8 blocks. Induction with vcr, pdn, asp, daunorubicine (dau) and intrathecal therapy (IT). Consolidation with ciclophosphamide (cfm), mercaptopurine (mp), cytarabine (cyt), vcr, asp and IT. CNS prophylaxis with methotrexate (mtx), followed by interim maintenance (im) combining vcr, mtx and asp. The other 4 blocks composed by delayed intensification (di) x 2 with vcr, dau, pdn, asp, cfm, mp, cyt, vcr and one im and di (as in induction). Hypercvad was prescribed with the addition of IT to each one of the 8 arms. Maintenance consisted of POMP for 2 years, and in some, combined with etoposide or anthracycline plus IT for 6 months. Rituximab (mab) was allowed at discretion if CD 20+. Ph+ cases received imatinib. Radiotherapy was permitted for mediastinal tumor. Patients changed the initial regimen if non hematological toxicity occurred during induction or by preference and registered in the regimen they continued. Variables analyzed: age (±30), WBC (≥30000 B and ≥100000 T), cytogenetic (t9;22 [ph+] and complex karyotypes), lineage, CD20, and aberrant markers. Relapse and death in CR due to toxicity were censored for the EFS analysis. Toxicity counted as one event in each block/arm (only ≥3 grade) or if admission or transfusion needed. Death during induction was excluded from the toxicity analysis.
Results
Fifty eight cases were treated. Median was 24 years (16-40). WBC was 15400 (0.6-632000). Twelve patients had karyotype and five were high risk (four ph+). Sixteen cases (33%) classified as high risk. Three cases had CNS disease. Fifty one (88%) cases were B and 48% CD 20+ (ten received mab). Seventeen had aberrant markers. Mediastinal tumor was observed in four T cell cases. The EFS of the whole group at 3 years was 30%. Forty five (78%) patients received induction with BFM with 8 deaths (17.7%), and thirteen (22%) with hypercvad with 2 deaths (15.3%). Median follow up was 12 months (1-72) with twenty one individuals in CR. Fourteen (29%) patients changed treatment, thirteen in the BFM group, 4 for pancreatitis and 9 by preference and one due to toxicity in the hypercvad group. Thirty three patients were included in BFM and twenty five in hypercvad. The EFS at three years was 32% for BFM and 28% for hypercvad p=.6. There were seventeen relapses (BFM 8 hypercvad 9) and ten deaths in CR due to toxicity (BFM 3 hypercvad 7). Toxic deaths in BFM were infectious in one and CNS toxicity in two. All toxic deaths in hypercvad were infectious Table 1. None of the variables had statistical difference. More toxic deaths occurred during the even courses and nearly 80% required admission for neutropenia and blood support (compared to a close 30% of the odd courses) in the hypercvad protocol. For the BFM, most admissions happened during consolidation (28%). The other blocks had less toxicity, although neurotoxicity occurred during maintenance. Mucositis presented barely in both groups. Coagulopathy and hepatitis rarely appeared with asp.
Conclusion
Both regimens had similar EFS but hypercvad had more deaths in CR due to myelotoxicity and more blood support and admission to the hospital. Severe non-myelotoxic events were uncommon.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Toxicity
Type: Eposter Presentation
Background
The experience to adapt pediatric protocols to adolescents and young adults (AYA) with acute lymphoblastic leukemia (ALL) is improving. Although there is still concern that toxicity may occur.
Aims
We present two groups of AYA treated with an adult protocol (hypercvad) and BFM developed for children. The study aimed to compare event free survival (EFS) and toxicity in both regimens.
Methods
Patients aged ≥16 and ≤40 between 2008-2015. BFM consisted of 8 blocks. Induction with vcr, pdn, asp, daunorubicine (dau) and intrathecal therapy (IT). Consolidation with ciclophosphamide (cfm), mercaptopurine (mp), cytarabine (cyt), vcr, asp and IT. CNS prophylaxis with methotrexate (mtx), followed by interim maintenance (im) combining vcr, mtx and asp. The other 4 blocks composed by delayed intensification (di) x 2 with vcr, dau, pdn, asp, cfm, mp, cyt, vcr and one im and di (as in induction). Hypercvad was prescribed with the addition of IT to each one of the 8 arms. Maintenance consisted of POMP for 2 years, and in some, combined with etoposide or anthracycline plus IT for 6 months. Rituximab (mab) was allowed at discretion if CD 20+. Ph+ cases received imatinib. Radiotherapy was permitted for mediastinal tumor. Patients changed the initial regimen if non hematological toxicity occurred during induction or by preference and registered in the regimen they continued. Variables analyzed: age (±30), WBC (≥30000 B and ≥100000 T), cytogenetic (t9;22 [ph+] and complex karyotypes), lineage, CD20, and aberrant markers. Relapse and death in CR due to toxicity were censored for the EFS analysis. Toxicity counted as one event in each block/arm (only ≥3 grade) or if admission or transfusion needed. Death during induction was excluded from the toxicity analysis.
Results
Fifty eight cases were treated. Median was 24 years (16-40). WBC was 15400 (0.6-632000). Twelve patients had karyotype and five were high risk (four ph+). Sixteen cases (33%) classified as high risk. Three cases had CNS disease. Fifty one (88%) cases were B and 48% CD 20+ (ten received mab). Seventeen had aberrant markers. Mediastinal tumor was observed in four T cell cases. The EFS of the whole group at 3 years was 30%. Forty five (78%) patients received induction with BFM with 8 deaths (17.7%), and thirteen (22%) with hypercvad with 2 deaths (15.3%). Median follow up was 12 months (1-72) with twenty one individuals in CR. Fourteen (29%) patients changed treatment, thirteen in the BFM group, 4 for pancreatitis and 9 by preference and one due to toxicity in the hypercvad group. Thirty three patients were included in BFM and twenty five in hypercvad. The EFS at three years was 32% for BFM and 28% for hypercvad p=.6. There were seventeen relapses (BFM 8 hypercvad 9) and ten deaths in CR due to toxicity (BFM 3 hypercvad 7). Toxic deaths in BFM were infectious in one and CNS toxicity in two. All toxic deaths in hypercvad were infectious Table 1. None of the variables had statistical difference. More toxic deaths occurred during the even courses and nearly 80% required admission for neutropenia and blood support (compared to a close 30% of the odd courses) in the hypercvad protocol. For the BFM, most admissions happened during consolidation (28%). The other blocks had less toxicity, although neurotoxicity occurred during maintenance. Mucositis presented barely in both groups. Coagulopathy and hepatitis rarely appeared with asp.
Conclusion
Both regimens had similar EFS but hypercvad had more deaths in CR due to myelotoxicity and more blood support and admission to the hospital. Severe non-myelotoxic events were uncommon.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, Toxicity
{{ help_message }}
{{filter}}


