DETAILED CHARACTERIZATION OF LAIP PROFILE AND HETEROGENEITY AT TIME OF DIAGNOSIS PREDICTS MINIMAL RESIDUAL DISEASE IN B-CELL PRECURSOR ALL
(Abstract release date: 05/19/16)
EHA Library. Modvig S. 06/09/16; 132407; E858
Disclosure(s): nothing to disclose

Dr. Signe Modvig
Contributions
Contributions
Abstract
Abstract: E858
Type: Eposter Presentation
Background
Early and accurate risk stratification in B-cell precursor acute lymphoblastic leukemia (BCP-ALL) is essential for individualized treatment strategies in order to improve prognosis and lower treatment associated toxicity. Leukemia-associated immunophenotype (LAIP) heterogeneity is common at time of diagnosis (Øbro et al, Leukemia, 2011) yet current immunophenotyping methods do not include heterogeneity. Furthermore, studies of the LAIP prognostic value have not shown consistent results.
Aims
To characterize in detail the LAIP and the frequency of immunophenotypically distinct subpopulations by flow cytometry at time of diagnosis and to evaluate their prognostic value for end-of-induction minimal residual disease (MRD) in BCP-ALL.
Methods
Flow cytometry data from time of diagnosis was re-evaluated retrospectively in 125 patients with BCP-ALL consecutively diagnosed between October 2011 and June 2015 and treated according to the NOPHO ALL 2008 protocol. The expression of intracellular and surface B-lineage markers (CD45, CD19, CD34, CD38, CD10, CD20, CD22, nTDT, cyCD79a, and cyCD22) and cross-lineage expressed markers (CD123, CD66c, CD133, CD13, CD33, and CD15) was scored as negative, positive dim, positive (normal) or positive bright, and broad or bimodal expression was registered. Corresponding normal populations in unaffected bone marrow samples were used as reference (methodological details will be presented). Groups were compared by the Mann-Whitney U test. The prognostic potential of LAIP expression was assessed in a multiple regression model with end-of-induction flow-MRD as outcome adjusting for age, WBC at diagnosis, cytogenetic group (high risk comprised hypodiploid, MLL, and iAMP21, non-high risk comprised t(12;21), hyperdiploid, t(1;19), dic(9;20), and no cytogenetic aberration) and NOPHO diagnostic treatment regime (high/standard risk).
Results
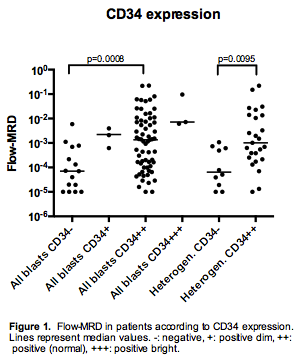
Distinct immunophenotypic subpopulations defined by bimodal expression of one or more markers were observed in 66 patients (53%), with nine patients (7%) having three or more subpopulations. The most frequently bimodal marker was CD34, displaying bimodality in 37 patients (30%).In patients with a homogeneous expression of CD34 we found higher end-of-induction flow-MRD in patients with CD34 positive blasts compared with CD34 negative (p=0.0008, figure 1). Accordingly, in patients with bimodal expression of CD34 we assessed the expression level of the dominant blast subpopulation and found that patients with a CD34 positive dominant blast subpopulation displayed higher end-of-induction MRD (p=0.0095, figure 1). When including all patients (CD34 homogeneous negative/dim/normal/bright and heterogeneous predominantly negative/positive) in an adjusted multiple regression model, we confirmed the prognostic value of CD34 score on MRD (p=0.0003).Since risk stratification of patients without identified cytogenetic aberrations is more difficult, we analyzed this subgroup separately, and found that CD34 expression is an independent predictor of high MRD (p=0.0074, multiple regression, n=37) in this group as well.
Conclusion
Detailed characterization of the CD34 expression level of blasts and immunophenotypically distinct subpopulations seems to bring valuable information on BCP-ALL prognosis regardless of age, WBC and cytogenetic findings. Detailed and standardized LAIP characterization is a readily accessible prognostic tool and could potentially be taken into consideration in future risk evaluations of BCP-ALL patients.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, CD34, Immunophenotype, Minimal residual disease (MRD)
Type: Eposter Presentation
Background
Early and accurate risk stratification in B-cell precursor acute lymphoblastic leukemia (BCP-ALL) is essential for individualized treatment strategies in order to improve prognosis and lower treatment associated toxicity. Leukemia-associated immunophenotype (LAIP) heterogeneity is common at time of diagnosis (Øbro et al, Leukemia, 2011) yet current immunophenotyping methods do not include heterogeneity. Furthermore, studies of the LAIP prognostic value have not shown consistent results.
Aims
To characterize in detail the LAIP and the frequency of immunophenotypically distinct subpopulations by flow cytometry at time of diagnosis and to evaluate their prognostic value for end-of-induction minimal residual disease (MRD) in BCP-ALL.
Methods
Flow cytometry data from time of diagnosis was re-evaluated retrospectively in 125 patients with BCP-ALL consecutively diagnosed between October 2011 and June 2015 and treated according to the NOPHO ALL 2008 protocol. The expression of intracellular and surface B-lineage markers (CD45, CD19, CD34, CD38, CD10, CD20, CD22, nTDT, cyCD79a, and cyCD22) and cross-lineage expressed markers (CD123, CD66c, CD133, CD13, CD33, and CD15) was scored as negative, positive dim, positive (normal) or positive bright, and broad or bimodal expression was registered. Corresponding normal populations in unaffected bone marrow samples were used as reference (methodological details will be presented). Groups were compared by the Mann-Whitney U test. The prognostic potential of LAIP expression was assessed in a multiple regression model with end-of-induction flow-MRD as outcome adjusting for age, WBC at diagnosis, cytogenetic group (high risk comprised hypodiploid, MLL, and iAMP21, non-high risk comprised t(12;21), hyperdiploid, t(1;19), dic(9;20), and no cytogenetic aberration) and NOPHO diagnostic treatment regime (high/standard risk).
Results
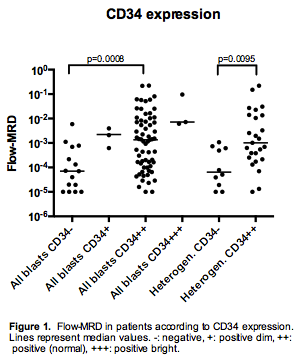
Distinct immunophenotypic subpopulations defined by bimodal expression of one or more markers were observed in 66 patients (53%), with nine patients (7%) having three or more subpopulations. The most frequently bimodal marker was CD34, displaying bimodality in 37 patients (30%).In patients with a homogeneous expression of CD34 we found higher end-of-induction flow-MRD in patients with CD34 positive blasts compared with CD34 negative (p=0.0008, figure 1). Accordingly, in patients with bimodal expression of CD34 we assessed the expression level of the dominant blast subpopulation and found that patients with a CD34 positive dominant blast subpopulation displayed higher end-of-induction MRD (p=0.0095, figure 1). When including all patients (CD34 homogeneous negative/dim/normal/bright and heterogeneous predominantly negative/positive) in an adjusted multiple regression model, we confirmed the prognostic value of CD34 score on MRD (p=0.0003).Since risk stratification of patients without identified cytogenetic aberrations is more difficult, we analyzed this subgroup separately, and found that CD34 expression is an independent predictor of high MRD (p=0.0074, multiple regression, n=37) in this group as well.
Conclusion
Detailed characterization of the CD34 expression level of blasts and immunophenotypically distinct subpopulations seems to bring valuable information on BCP-ALL prognosis regardless of age, WBC and cytogenetic findings. Detailed and standardized LAIP characterization is a readily accessible prognostic tool and could potentially be taken into consideration in future risk evaluations of BCP-ALL patients.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, CD34, Immunophenotype, Minimal residual disease (MRD)
Abstract: E858
Type: Eposter Presentation
Background
Early and accurate risk stratification in B-cell precursor acute lymphoblastic leukemia (BCP-ALL) is essential for individualized treatment strategies in order to improve prognosis and lower treatment associated toxicity. Leukemia-associated immunophenotype (LAIP) heterogeneity is common at time of diagnosis (Øbro et al, Leukemia, 2011) yet current immunophenotyping methods do not include heterogeneity. Furthermore, studies of the LAIP prognostic value have not shown consistent results.
Aims
To characterize in detail the LAIP and the frequency of immunophenotypically distinct subpopulations by flow cytometry at time of diagnosis and to evaluate their prognostic value for end-of-induction minimal residual disease (MRD) in BCP-ALL.
Methods
Flow cytometry data from time of diagnosis was re-evaluated retrospectively in 125 patients with BCP-ALL consecutively diagnosed between October 2011 and June 2015 and treated according to the NOPHO ALL 2008 protocol. The expression of intracellular and surface B-lineage markers (CD45, CD19, CD34, CD38, CD10, CD20, CD22, nTDT, cyCD79a, and cyCD22) and cross-lineage expressed markers (CD123, CD66c, CD133, CD13, CD33, and CD15) was scored as negative, positive dim, positive (normal) or positive bright, and broad or bimodal expression was registered. Corresponding normal populations in unaffected bone marrow samples were used as reference (methodological details will be presented). Groups were compared by the Mann-Whitney U test. The prognostic potential of LAIP expression was assessed in a multiple regression model with end-of-induction flow-MRD as outcome adjusting for age, WBC at diagnosis, cytogenetic group (high risk comprised hypodiploid, MLL, and iAMP21, non-high risk comprised t(12;21), hyperdiploid, t(1;19), dic(9;20), and no cytogenetic aberration) and NOPHO diagnostic treatment regime (high/standard risk).
Results
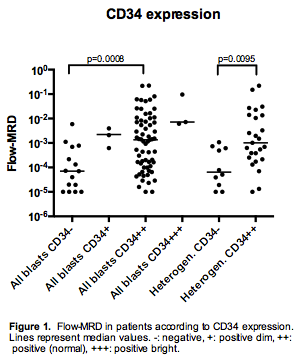
Distinct immunophenotypic subpopulations defined by bimodal expression of one or more markers were observed in 66 patients (53%), with nine patients (7%) having three or more subpopulations. The most frequently bimodal marker was CD34, displaying bimodality in 37 patients (30%).In patients with a homogeneous expression of CD34 we found higher end-of-induction flow-MRD in patients with CD34 positive blasts compared with CD34 negative (p=0.0008, figure 1). Accordingly, in patients with bimodal expression of CD34 we assessed the expression level of the dominant blast subpopulation and found that patients with a CD34 positive dominant blast subpopulation displayed higher end-of-induction MRD (p=0.0095, figure 1). When including all patients (CD34 homogeneous negative/dim/normal/bright and heterogeneous predominantly negative/positive) in an adjusted multiple regression model, we confirmed the prognostic value of CD34 score on MRD (p=0.0003).Since risk stratification of patients without identified cytogenetic aberrations is more difficult, we analyzed this subgroup separately, and found that CD34 expression is an independent predictor of high MRD (p=0.0074, multiple regression, n=37) in this group as well.
Conclusion
Detailed characterization of the CD34 expression level of blasts and immunophenotypically distinct subpopulations seems to bring valuable information on BCP-ALL prognosis regardless of age, WBC and cytogenetic findings. Detailed and standardized LAIP characterization is a readily accessible prognostic tool and could potentially be taken into consideration in future risk evaluations of BCP-ALL patients.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, CD34, Immunophenotype, Minimal residual disease (MRD)
Type: Eposter Presentation
Background
Early and accurate risk stratification in B-cell precursor acute lymphoblastic leukemia (BCP-ALL) is essential for individualized treatment strategies in order to improve prognosis and lower treatment associated toxicity. Leukemia-associated immunophenotype (LAIP) heterogeneity is common at time of diagnosis (Øbro et al, Leukemia, 2011) yet current immunophenotyping methods do not include heterogeneity. Furthermore, studies of the LAIP prognostic value have not shown consistent results.
Aims
To characterize in detail the LAIP and the frequency of immunophenotypically distinct subpopulations by flow cytometry at time of diagnosis and to evaluate their prognostic value for end-of-induction minimal residual disease (MRD) in BCP-ALL.
Methods
Flow cytometry data from time of diagnosis was re-evaluated retrospectively in 125 patients with BCP-ALL consecutively diagnosed between October 2011 and June 2015 and treated according to the NOPHO ALL 2008 protocol. The expression of intracellular and surface B-lineage markers (CD45, CD19, CD34, CD38, CD10, CD20, CD22, nTDT, cyCD79a, and cyCD22) and cross-lineage expressed markers (CD123, CD66c, CD133, CD13, CD33, and CD15) was scored as negative, positive dim, positive (normal) or positive bright, and broad or bimodal expression was registered. Corresponding normal populations in unaffected bone marrow samples were used as reference (methodological details will be presented). Groups were compared by the Mann-Whitney U test. The prognostic potential of LAIP expression was assessed in a multiple regression model with end-of-induction flow-MRD as outcome adjusting for age, WBC at diagnosis, cytogenetic group (high risk comprised hypodiploid, MLL, and iAMP21, non-high risk comprised t(12;21), hyperdiploid, t(1;19), dic(9;20), and no cytogenetic aberration) and NOPHO diagnostic treatment regime (high/standard risk).
Results
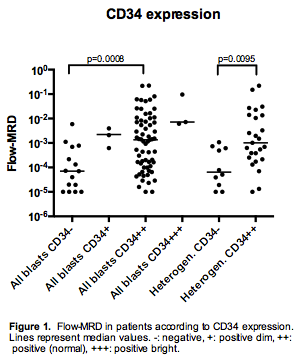
Distinct immunophenotypic subpopulations defined by bimodal expression of one or more markers were observed in 66 patients (53%), with nine patients (7%) having three or more subpopulations. The most frequently bimodal marker was CD34, displaying bimodality in 37 patients (30%).In patients with a homogeneous expression of CD34 we found higher end-of-induction flow-MRD in patients with CD34 positive blasts compared with CD34 negative (p=0.0008, figure 1). Accordingly, in patients with bimodal expression of CD34 we assessed the expression level of the dominant blast subpopulation and found that patients with a CD34 positive dominant blast subpopulation displayed higher end-of-induction MRD (p=0.0095, figure 1). When including all patients (CD34 homogeneous negative/dim/normal/bright and heterogeneous predominantly negative/positive) in an adjusted multiple regression model, we confirmed the prognostic value of CD34 score on MRD (p=0.0003).Since risk stratification of patients without identified cytogenetic aberrations is more difficult, we analyzed this subgroup separately, and found that CD34 expression is an independent predictor of high MRD (p=0.0074, multiple regression, n=37) in this group as well.
Conclusion
Detailed characterization of the CD34 expression level of blasts and immunophenotypically distinct subpopulations seems to bring valuable information on BCP-ALL prognosis regardless of age, WBC and cytogenetic findings. Detailed and standardized LAIP characterization is a readily accessible prognostic tool and could potentially be taken into consideration in future risk evaluations of BCP-ALL patients.
Session topic: E-poster
Keyword(s): Acute lymphoblastic leukemia, CD34, Immunophenotype, Minimal residual disease (MRD)
{{ help_message }}
{{filter}}


