ACCURACY OF PHYSICIAN ASSESSMENT OF TREATMENT PREFERENCES AND HEALTH STATUS IN PATIENTS WITH HIGHER-RISK MYELODYSPLASTIC SYNDROMES
(Abstract release date: 05/21/15)
EHA Library. Caocci G. 06/12/15; 103103; S147

Dr. Giovanni Caocci
Contributions
Contributions
Abstract
Abstract: S147
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 11:45 to 12.06.2015 12:00
Location: Room Stolz 2
Background
Higher-risk myelodysplastic syndromes (MDS) are rarely curable and have a poor prognosis, with short life expectancy. Thus it becomes essential for physicians to accurately evaluate the patients’ wishes and preferences in light of the risks, benefits and appropriateness of treatment.
Aims
The primary aim was to investigate the accuracy of physicians’ perception of patients’ health status and the patients’ preferences for involvement in treatment decisions. A secondary objective was to investigate physicians’ attitude toward patient involvement in treatment decisions and to examine factors influencing physicians to be more patient inclusive or exclusive in the shared decision-making process.
Methods
We investigated 280 high-risk MDS patients paired with 68 physicians to evaluate physician-patient agreement on preferences for involvement in treatment decisions and self-reported health status. Control Preferences Scale (CPS) and the questionnaire EORTC QLQ-C30 were used to evaluate these parameters, respectively. Simple and weighted κ-coefficient was used to assess the degree of physician-patient agreement. The following variables were ascertained: physician gender and age; the overall number of years in practice; the number of years of experience in treating MDS patients.
Results
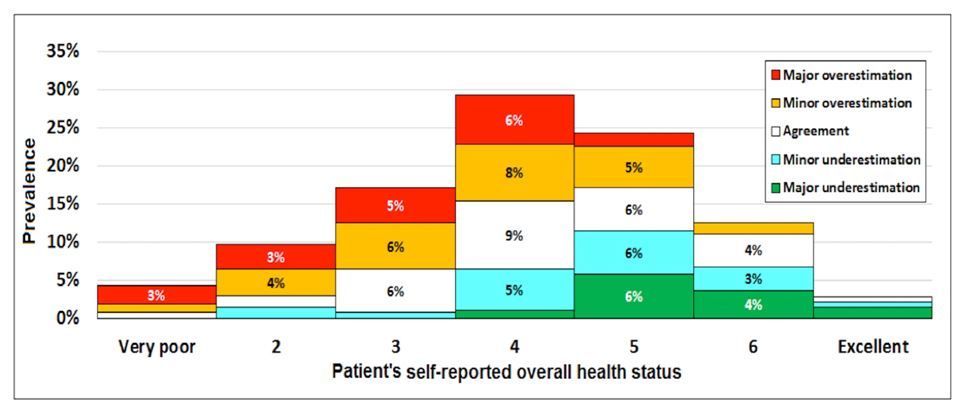
The median age of the physicians was 44 years (range 28-64) and their median duration of medical practice was 16 years, with a median of 11 years of expertise in MDS. Analysis was based on 280 patient-physician dyads. Overall concordance was 49% for physician perception of patient preferences for involvement in treatment decisions, with a weighted K-coefficient indicating poor concordance. In 36.4% of comparisons there were minor differences and in 14.6% there were major differences. In 44.7% of the patients preferring a passive role, physicians perceived them as preferring an active or collaborative role. The only factors independently associated with the physicians’ attitude toward less involvement of their patients in clinical decisions were absence of the patient’s request for prognostic information (P=0.001) and judging the patient as having a poor health status (P=0.036). The degree of agreement between physicians and patients in evaluating overall health status was low. Agreement on health status was found in 27.5% of cases. Physicians most frequently tended to overestimate health status of patients who reported low-level health status (Figure).
Summary
Physicians treating MDS patients often have difficulty in understanding what their patients’ preferences are and some do not consider the patients’ preferences to be important. General concordance on physicians’ perception and patients’ health status was present in slightly less than one third of comparisons. In particular, physicians tended to overestimate the health status of patients reporting low levels for this parameter. Physicians need to improve their perception of patients’ health status in view of the important implications associated with assessment of patient eligibility for inclusion in clinical trials. Moreover, clinicians need to be provided with decision aid tools that can improve their perceptions and communication skills.
Keyword(s): Hematological malignancy, Myelodysplasia, Quality of life
Session topic: Quality of life and health economics
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 11:45 to 12.06.2015 12:00
Location: Room Stolz 2
Background
Higher-risk myelodysplastic syndromes (MDS) are rarely curable and have a poor prognosis, with short life expectancy. Thus it becomes essential for physicians to accurately evaluate the patients’ wishes and preferences in light of the risks, benefits and appropriateness of treatment.
Aims
The primary aim was to investigate the accuracy of physicians’ perception of patients’ health status and the patients’ preferences for involvement in treatment decisions. A secondary objective was to investigate physicians’ attitude toward patient involvement in treatment decisions and to examine factors influencing physicians to be more patient inclusive or exclusive in the shared decision-making process.
Methods
We investigated 280 high-risk MDS patients paired with 68 physicians to evaluate physician-patient agreement on preferences for involvement in treatment decisions and self-reported health status. Control Preferences Scale (CPS) and the questionnaire EORTC QLQ-C30 were used to evaluate these parameters, respectively. Simple and weighted κ-coefficient was used to assess the degree of physician-patient agreement. The following variables were ascertained: physician gender and age; the overall number of years in practice; the number of years of experience in treating MDS patients.
Results
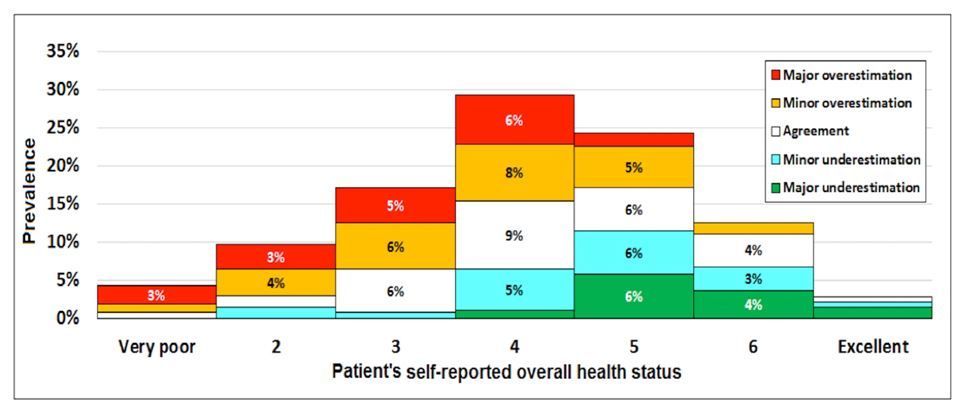
The median age of the physicians was 44 years (range 28-64) and their median duration of medical practice was 16 years, with a median of 11 years of expertise in MDS. Analysis was based on 280 patient-physician dyads. Overall concordance was 49% for physician perception of patient preferences for involvement in treatment decisions, with a weighted K-coefficient indicating poor concordance. In 36.4% of comparisons there were minor differences and in 14.6% there were major differences. In 44.7% of the patients preferring a passive role, physicians perceived them as preferring an active or collaborative role. The only factors independently associated with the physicians’ attitude toward less involvement of their patients in clinical decisions were absence of the patient’s request for prognostic information (P=0.001) and judging the patient as having a poor health status (P=0.036). The degree of agreement between physicians and patients in evaluating overall health status was low. Agreement on health status was found in 27.5% of cases. Physicians most frequently tended to overestimate health status of patients who reported low-level health status (Figure).
Summary
Physicians treating MDS patients often have difficulty in understanding what their patients’ preferences are and some do not consider the patients’ preferences to be important. General concordance on physicians’ perception and patients’ health status was present in slightly less than one third of comparisons. In particular, physicians tended to overestimate the health status of patients reporting low levels for this parameter. Physicians need to improve their perception of patients’ health status in view of the important implications associated with assessment of patient eligibility for inclusion in clinical trials. Moreover, clinicians need to be provided with decision aid tools that can improve their perceptions and communication skills.
Keyword(s): Hematological malignancy, Myelodysplasia, Quality of life
Session topic: Quality of life and health economics
Abstract: S147
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 11:45 to 12.06.2015 12:00
Location: Room Stolz 2
Background
Higher-risk myelodysplastic syndromes (MDS) are rarely curable and have a poor prognosis, with short life expectancy. Thus it becomes essential for physicians to accurately evaluate the patients’ wishes and preferences in light of the risks, benefits and appropriateness of treatment.
Aims
The primary aim was to investigate the accuracy of physicians’ perception of patients’ health status and the patients’ preferences for involvement in treatment decisions. A secondary objective was to investigate physicians’ attitude toward patient involvement in treatment decisions and to examine factors influencing physicians to be more patient inclusive or exclusive in the shared decision-making process.
Methods
We investigated 280 high-risk MDS patients paired with 68 physicians to evaluate physician-patient agreement on preferences for involvement in treatment decisions and self-reported health status. Control Preferences Scale (CPS) and the questionnaire EORTC QLQ-C30 were used to evaluate these parameters, respectively. Simple and weighted κ-coefficient was used to assess the degree of physician-patient agreement. The following variables were ascertained: physician gender and age; the overall number of years in practice; the number of years of experience in treating MDS patients.
Results
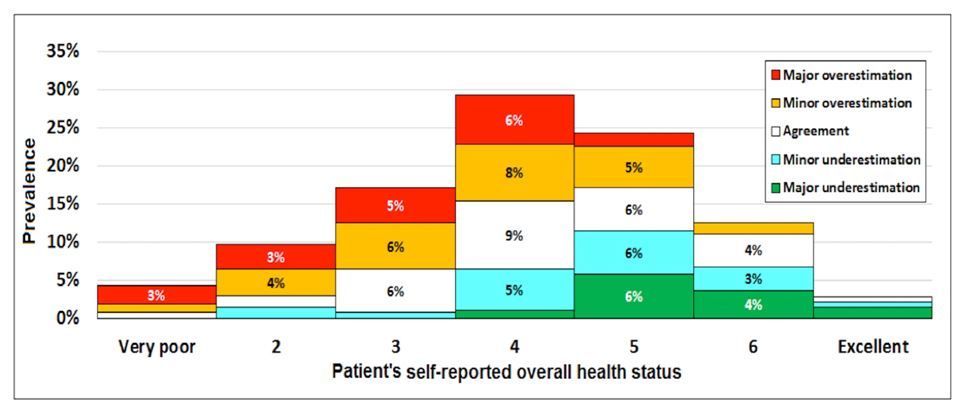
The median age of the physicians was 44 years (range 28-64) and their median duration of medical practice was 16 years, with a median of 11 years of expertise in MDS. Analysis was based on 280 patient-physician dyads. Overall concordance was 49% for physician perception of patient preferences for involvement in treatment decisions, with a weighted K-coefficient indicating poor concordance. In 36.4% of comparisons there were minor differences and in 14.6% there were major differences. In 44.7% of the patients preferring a passive role, physicians perceived them as preferring an active or collaborative role. The only factors independently associated with the physicians’ attitude toward less involvement of their patients in clinical decisions were absence of the patient’s request for prognostic information (P=0.001) and judging the patient as having a poor health status (P=0.036). The degree of agreement between physicians and patients in evaluating overall health status was low. Agreement on health status was found in 27.5% of cases. Physicians most frequently tended to overestimate health status of patients who reported low-level health status (Figure).
Summary
Physicians treating MDS patients often have difficulty in understanding what their patients’ preferences are and some do not consider the patients’ preferences to be important. General concordance on physicians’ perception and patients’ health status was present in slightly less than one third of comparisons. In particular, physicians tended to overestimate the health status of patients reporting low levels for this parameter. Physicians need to improve their perception of patients’ health status in view of the important implications associated with assessment of patient eligibility for inclusion in clinical trials. Moreover, clinicians need to be provided with decision aid tools that can improve their perceptions and communication skills.
Keyword(s): Hematological malignancy, Myelodysplasia, Quality of life
Session topic: Quality of life and health economics
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 11:45 to 12.06.2015 12:00
Location: Room Stolz 2
Background
Higher-risk myelodysplastic syndromes (MDS) are rarely curable and have a poor prognosis, with short life expectancy. Thus it becomes essential for physicians to accurately evaluate the patients’ wishes and preferences in light of the risks, benefits and appropriateness of treatment.
Aims
The primary aim was to investigate the accuracy of physicians’ perception of patients’ health status and the patients’ preferences for involvement in treatment decisions. A secondary objective was to investigate physicians’ attitude toward patient involvement in treatment decisions and to examine factors influencing physicians to be more patient inclusive or exclusive in the shared decision-making process.
Methods
We investigated 280 high-risk MDS patients paired with 68 physicians to evaluate physician-patient agreement on preferences for involvement in treatment decisions and self-reported health status. Control Preferences Scale (CPS) and the questionnaire EORTC QLQ-C30 were used to evaluate these parameters, respectively. Simple and weighted κ-coefficient was used to assess the degree of physician-patient agreement. The following variables were ascertained: physician gender and age; the overall number of years in practice; the number of years of experience in treating MDS patients.
Results
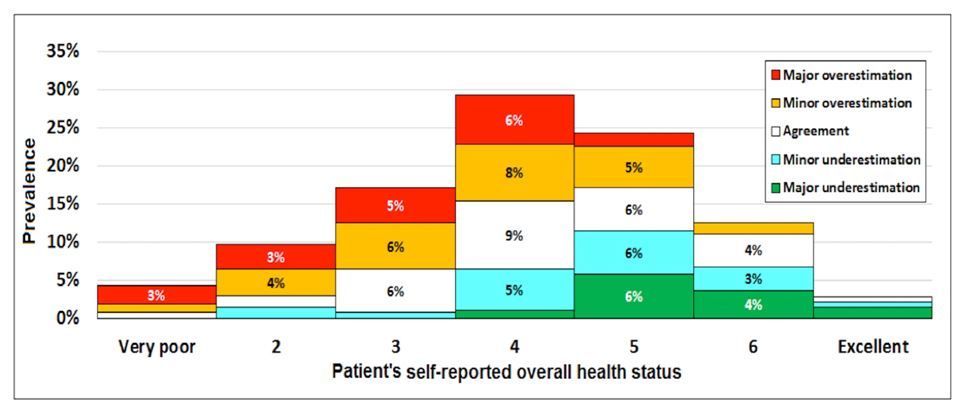
The median age of the physicians was 44 years (range 28-64) and their median duration of medical practice was 16 years, with a median of 11 years of expertise in MDS. Analysis was based on 280 patient-physician dyads. Overall concordance was 49% for physician perception of patient preferences for involvement in treatment decisions, with a weighted K-coefficient indicating poor concordance. In 36.4% of comparisons there were minor differences and in 14.6% there were major differences. In 44.7% of the patients preferring a passive role, physicians perceived them as preferring an active or collaborative role. The only factors independently associated with the physicians’ attitude toward less involvement of their patients in clinical decisions were absence of the patient’s request for prognostic information (P=0.001) and judging the patient as having a poor health status (P=0.036). The degree of agreement between physicians and patients in evaluating overall health status was low. Agreement on health status was found in 27.5% of cases. Physicians most frequently tended to overestimate health status of patients who reported low-level health status (Figure).
Summary
Physicians treating MDS patients often have difficulty in understanding what their patients’ preferences are and some do not consider the patients’ preferences to be important. General concordance on physicians’ perception and patients’ health status was present in slightly less than one third of comparisons. In particular, physicians tended to overestimate the health status of patients reporting low levels for this parameter. Physicians need to improve their perception of patients’ health status in view of the important implications associated with assessment of patient eligibility for inclusion in clinical trials. Moreover, clinicians need to be provided with decision aid tools that can improve their perceptions and communication skills.
Keyword(s): Hematological malignancy, Myelodysplasia, Quality of life
Session topic: Quality of life and health economics
{{ help_message }}
{{filter}}


