
Contributions
Type: Oral Presentation
Presentation during EHA20: From 13.06.2015 16:45 to 13.06.2015 17:00
Location: Room A8
Background
For patients (pts) with CML, achieving and maintaining a deep molecular response (MR4 ≤0.01% or MR4.5 ≤0.0032%) is necessary to minimize the risk of relapse after tyrosine kinase inhibitor (TKI) discontinuation, which is desirable for long term management of side effects, pregnancy and for economic reasons. For most pts, TKI therapy achieves an initial rapid BCR-ABL reduction, followed by a slow decline over many years. Thus, attaining a deep molecular response requires a long time. More potent TKIs administered as first line or after switch from imatinib (IM) yield higher rates of MR4.5. IM treated pts who switched to nilotinib were indeed more likely to achieve MR4.5 in the subsequent 2 years compared to continuing on IM (Hughes Blood 2014). However, decisions on treatment switch warrant careful consideration for a responding patient tolerating IM, who risks toxicity of second-line therapy. We analyzed BCR-ABL levels during IM therapy to determine the probability and timing of subsequent deep molecular response. This information could guide decisions on treatment switch if certain BCR-ABL response levels are associated with slow achievement of deep molecular response.
Aims
We 1) determined the probability of achieving MR4 or MR4.5 on IM, based on BCR-ABL levels attained; 2) assessed the time to reach these responses; and 3) identified subgroups where a switch to a more potent TKI may be warranted if timely TKI discontinuation is the goal.
Methods
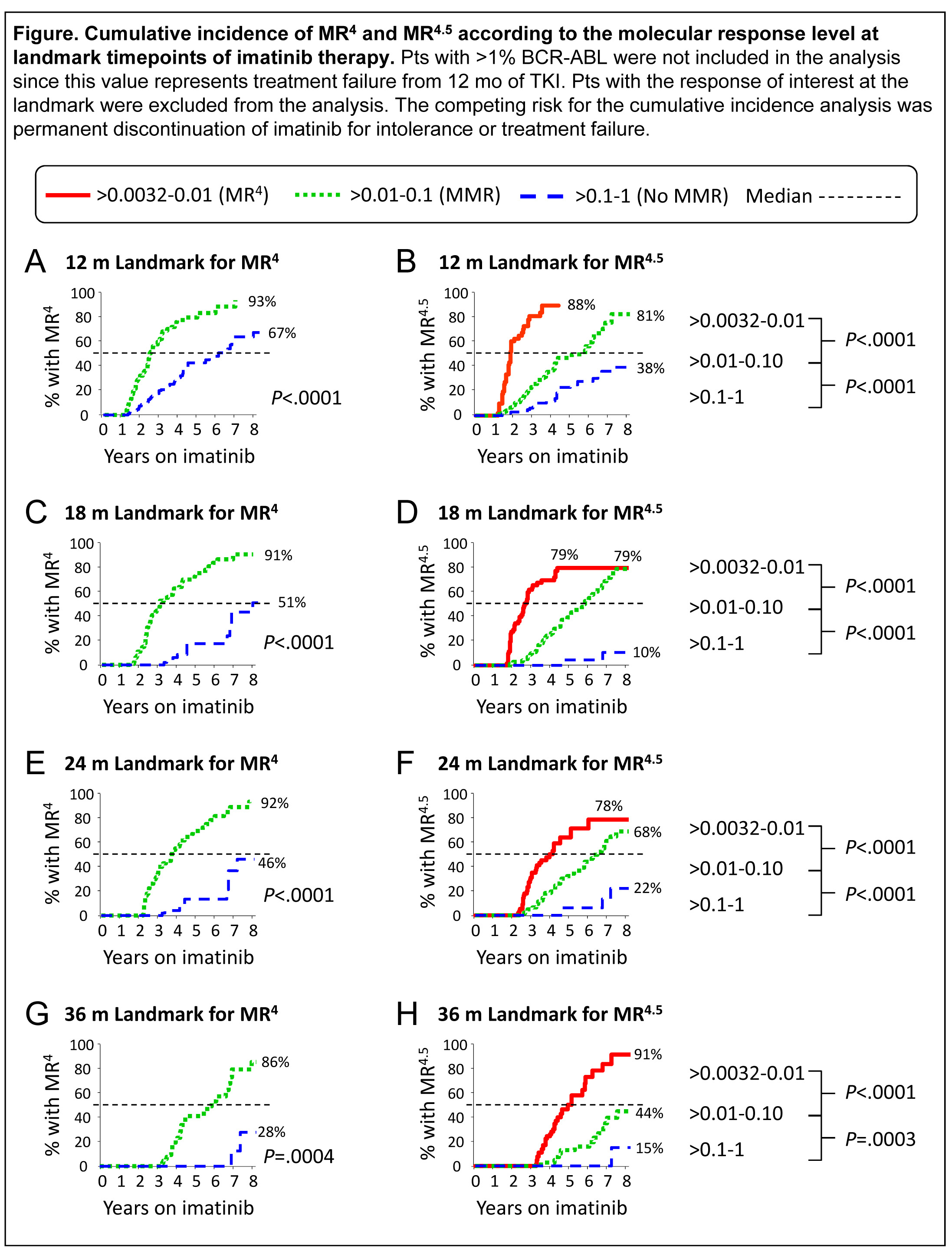
528 consecutive first line IM treated pts were examined. Pts were grouped by their BCR-ABL level at 12, 18, 24 and 36 months (mo) of IM and cumulative incidence of confirmed MR4 and MR4.5 by 8 years were calculated. The BCR-ABL groups were >0.01-0.1% and >0.1-1% for subsequent achievement of MR4, and >0.0032-0.01%, >0.01-0.1% and >0.1-1% for MR4.5.
Results
By 8 years, the overall cumulative incidence of MR4 and MR4.5 were 66% and 53%. At landmark timepoints the subsequent rates of MR4 or MR4.5 were significantly associated with the BCR-ABL level, Figure. Rates at 8 years ranged from 91% MR4.5 for pts with >0.0032-0.01% (MR4) at 36 mo to 15% MR4.5 for pts with >0.1-1% (no MMR) at 36 mo, P<.0001. The majority of pts with MR4 at any of the landmarks achieved MR4.5 within the subsequent 2 years with continued IM. The median time to achieve MR4.5 for pts without an MMR at ≥12 mo was not reached with up to 7 additional years of IM. A substantial temporal lag in attaining the deep molecular responses was evident between the BCR-ABL groups for each landmark analysis. For example, for patients with MR4 at 12 mo the median time to MR4.5 was 23 mo after start of IM. However, for pts with BCR-ABL >0.01-0.1% at 12 mo (MMR) the median time to MR4.5 was 69 mo after start of IM, a difference of >3.5 years (Fig B).
Summary
BCR-ABL levels are a powerful predictor of long term response. Whether switching therapy to achieve timely deep response will be associated with higher rates of treatment free remission compared with continuing on IM is currently unknown. Nevertheless, our data show that pts with <1% BCR-ABL without an MMR by 18-36 mo have a low chance of attaining MR4.5, even with up to 6.5 additional years of IM, whereas most pts with MR4 at any time achieved MR4.5 with ~2 additional years of IM. These data provide timelines for the achievement of molecular response levels to clinicians and their IM-treated pts, and will guide decisions for potential therapy switch to optimise TKI discontinuation opportunities in pts where this is the goal of long term management.
Keyword(s): BCR-ABL, Molecular response
Session topic: CML: Clinical trials
Type: Oral Presentation
Presentation during EHA20: From 13.06.2015 16:45 to 13.06.2015 17:00
Location: Room A8
Background
For patients (pts) with CML, achieving and maintaining a deep molecular response (MR4 ≤0.01% or MR4.5 ≤0.0032%) is necessary to minimize the risk of relapse after tyrosine kinase inhibitor (TKI) discontinuation, which is desirable for long term management of side effects, pregnancy and for economic reasons. For most pts, TKI therapy achieves an initial rapid BCR-ABL reduction, followed by a slow decline over many years. Thus, attaining a deep molecular response requires a long time. More potent TKIs administered as first line or after switch from imatinib (IM) yield higher rates of MR4.5. IM treated pts who switched to nilotinib were indeed more likely to achieve MR4.5 in the subsequent 2 years compared to continuing on IM (Hughes Blood 2014). However, decisions on treatment switch warrant careful consideration for a responding patient tolerating IM, who risks toxicity of second-line therapy. We analyzed BCR-ABL levels during IM therapy to determine the probability and timing of subsequent deep molecular response. This information could guide decisions on treatment switch if certain BCR-ABL response levels are associated with slow achievement of deep molecular response.
Aims
We 1) determined the probability of achieving MR4 or MR4.5 on IM, based on BCR-ABL levels attained; 2) assessed the time to reach these responses; and 3) identified subgroups where a switch to a more potent TKI may be warranted if timely TKI discontinuation is the goal.
Methods
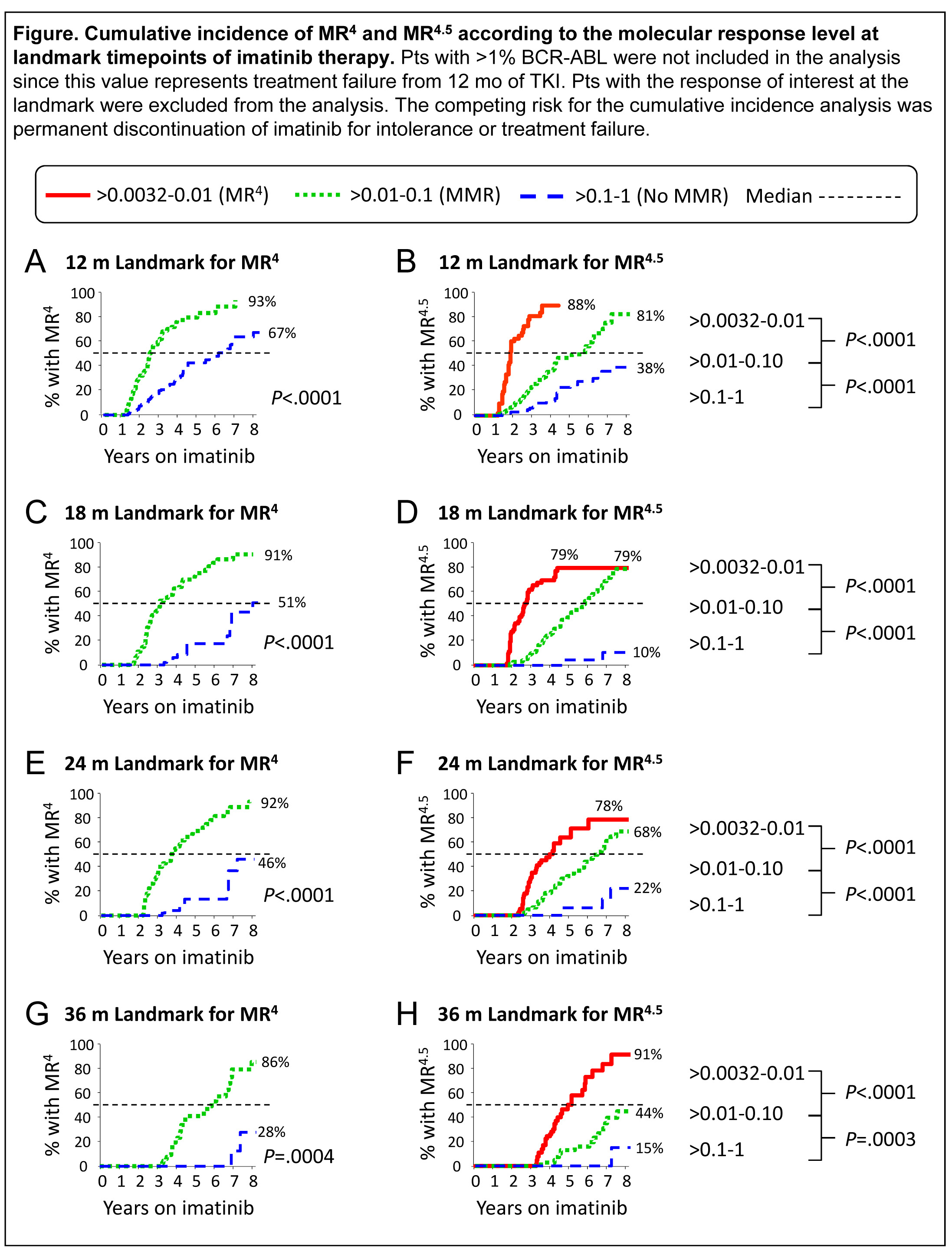
528 consecutive first line IM treated pts were examined. Pts were grouped by their BCR-ABL level at 12, 18, 24 and 36 months (mo) of IM and cumulative incidence of confirmed MR4 and MR4.5 by 8 years were calculated. The BCR-ABL groups were >0.01-0.1% and >0.1-1% for subsequent achievement of MR4, and >0.0032-0.01%, >0.01-0.1% and >0.1-1% for MR4.5.
Results
By 8 years, the overall cumulative incidence of MR4 and MR4.5 were 66% and 53%. At landmark timepoints the subsequent rates of MR4 or MR4.5 were significantly associated with the BCR-ABL level, Figure. Rates at 8 years ranged from 91% MR4.5 for pts with >0.0032-0.01% (MR4) at 36 mo to 15% MR4.5 for pts with >0.1-1% (no MMR) at 36 mo, P<.0001. The majority of pts with MR4 at any of the landmarks achieved MR4.5 within the subsequent 2 years with continued IM. The median time to achieve MR4.5 for pts without an MMR at ≥12 mo was not reached with up to 7 additional years of IM. A substantial temporal lag in attaining the deep molecular responses was evident between the BCR-ABL groups for each landmark analysis. For example, for patients with MR4 at 12 mo the median time to MR4.5 was 23 mo after start of IM. However, for pts with BCR-ABL >0.01-0.1% at 12 mo (MMR) the median time to MR4.5 was 69 mo after start of IM, a difference of >3.5 years (Fig B).
Summary
BCR-ABL levels are a powerful predictor of long term response. Whether switching therapy to achieve timely deep response will be associated with higher rates of treatment free remission compared with continuing on IM is currently unknown. Nevertheless, our data show that pts with <1% BCR-ABL without an MMR by 18-36 mo have a low chance of attaining MR4.5, even with up to 6.5 additional years of IM, whereas most pts with MR4 at any time achieved MR4.5 with ~2 additional years of IM. These data provide timelines for the achievement of molecular response levels to clinicians and their IM-treated pts, and will guide decisions for potential therapy switch to optimise TKI discontinuation opportunities in pts where this is the goal of long term management.
Keyword(s): BCR-ABL, Molecular response
Session topic: CML: Clinical trials


