
Contributions
Type: Oral Presentation
Presentation during EHA20: From 13.06.2015 16:30 to 13.06.2015 16:45
Location: Room A7
Background
A significant proportion of primary CNS lymphoma (PCNSL) patients is refractory or relapses after first line therapy. Clinical presentation and therapeutic management of patients with relapsed/refractory (R/R) PCNSL are heterogeneous.
Aims
The aim of this study was to analyze the characteristics, management, and outcome of R/R PCNSL patients after first-line therapy.
Methods
We analyzed patients with R/R PCNSL who had been prospectively registered in the database of the French LOC network between 2011 and 2014.
Results
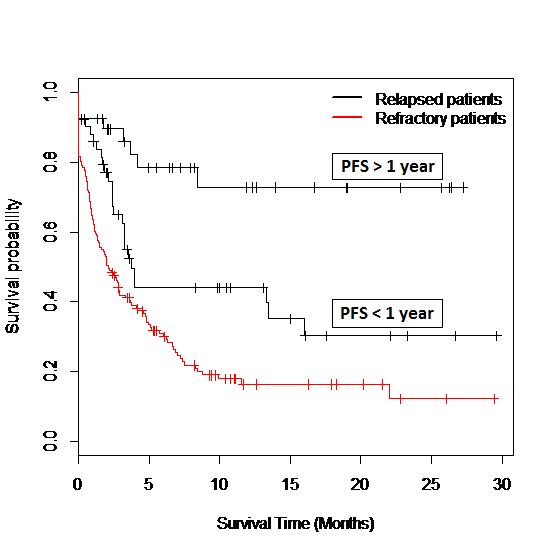
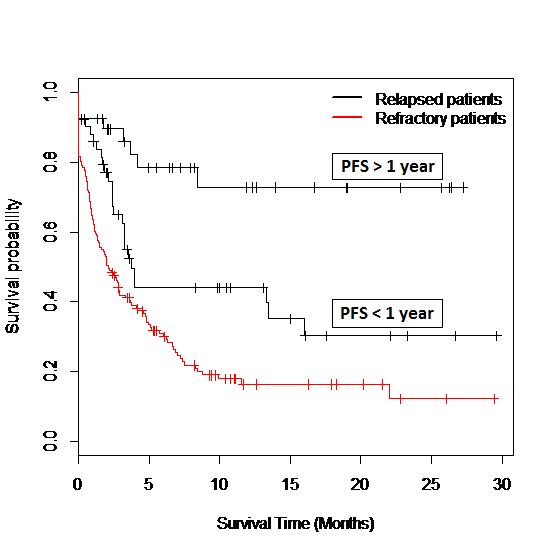
Among 563 PCNSL patients registered in the LOC database, we identified 256 patients with relapsed (N=93, 16.5%) or refractory (N=163, 29.0%) disease after a median follow-up of 9 [0.3-43.0] months. Median age was 68 [26-93] years. Most patients (92.6%) had received a methotrexate-based chemotherapy as first line treatment. First relapse/progression occurred after a median progression-free survival from diagnosis (PFS1) of 5.1 [0.3-35.8] months. Relapse/progression was asymptomatic in 25.5% of the cases, mostly diagnosed on systematic neuroimaging. Overall survival after relapse/progression (OS2) was 3.5 [0-29.6] months for the entire cohort. At first relapse/progression, 28.2% of the patients received palliative care. All of them died within 5 months with a median OS2 of 0.6 months. The remaining patients (71.8%) received salvage chemotherapy (methotrexate, cytarabine or ifosfamide-based regimens) without (79.5%) or with (20.5%) consolidation therapy consisting in radiotherapy (14.7%) or intensive chemotherapy followed by autologous stem cell transplantation (ICT+ASCT) (85.3%). Survival was significantly longer in patients receiving consolidation therapy with a median PFS2 (PFS from first relapse/progression) of 13.5 vs 2.6 months and a median OS2 not reached vs 6.7 months (p<0.01). In patients receiving ICT+ASCT, 44.8% (13/29) experienced a PFS2 longer than their PFS1. Survival was significantly worse in refractory patients and in relapsed patients with a PFS1<1 year (median OS2 = 2.1 and 3.7 months, respectively) compared to relapsed patients with a PFS1>1 year (median OS2 not reached, p<0.01)(Figure 1). Other prognostic factors were age (< vs > 60 years), Karnofsky index (KI, > vs < 70%), administration of a salvage therapy, and administration of Rituximab. In multivariate analysis, three prognostic factors remained statistically independent: performance status (KI), duration of first remission (PFS1) and administration of a salvage therapy.
Summary
One fourth of R/R PCNSL are asymptomatic underlining the need for systematic neuroimaging in surveillance. Duration of first remission (PFS1) is a strong prognostic factor. Salvage chemotherapy followed by consolidation with ICT+ASCT is associated with prolonged remission in a subset of patients.
Keyword(s): CNS lymphoma
Session topic: Optimization and innovation in treating aggressive lymphomas
Type: Oral Presentation
Presentation during EHA20: From 13.06.2015 16:30 to 13.06.2015 16:45
Location: Room A7
Background
A significant proportion of primary CNS lymphoma (PCNSL) patients is refractory or relapses after first line therapy. Clinical presentation and therapeutic management of patients with relapsed/refractory (R/R) PCNSL are heterogeneous.
Aims
The aim of this study was to analyze the characteristics, management, and outcome of R/R PCNSL patients after first-line therapy.
Methods
We analyzed patients with R/R PCNSL who had been prospectively registered in the database of the French LOC network between 2011 and 2014.
Results
Among 563 PCNSL patients registered in the LOC database, we identified 256 patients with relapsed (N=93, 16.5%) or refractory (N=163, 29.0%) disease after a median follow-up of 9 [0.3-43.0] months. Median age was 68 [26-93] years. Most patients (92.6%) had received a methotrexate-based chemotherapy as first line treatment. First relapse/progression occurred after a median progression-free survival from diagnosis (PFS1) of 5.1 [0.3-35.8] months. Relapse/progression was asymptomatic in 25.5% of the cases, mostly diagnosed on systematic neuroimaging. Overall survival after relapse/progression (OS2) was 3.5 [0-29.6] months for the entire cohort. At first relapse/progression, 28.2% of the patients received palliative care. All of them died within 5 months with a median OS2 of 0.6 months. The remaining patients (71.8%) received salvage chemotherapy (methotrexate, cytarabine or ifosfamide-based regimens) without (79.5%) or with (20.5%) consolidation therapy consisting in radiotherapy (14.7%) or intensive chemotherapy followed by autologous stem cell transplantation (ICT+ASCT) (85.3%). Survival was significantly longer in patients receiving consolidation therapy with a median PFS2 (PFS from first relapse/progression) of 13.5 vs 2.6 months and a median OS2 not reached vs 6.7 months (p<0.01). In patients receiving ICT+ASCT, 44.8% (13/29) experienced a PFS2 longer than their PFS1. Survival was significantly worse in refractory patients and in relapsed patients with a PFS1<1 year (median OS2 = 2.1 and 3.7 months, respectively) compared to relapsed patients with a PFS1>1 year (median OS2 not reached, p<0.01)(Figure 1). Other prognostic factors were age (< vs > 60 years), Karnofsky index (KI, > vs < 70%), administration of a salvage therapy, and administration of Rituximab. In multivariate analysis, three prognostic factors remained statistically independent: performance status (KI), duration of first remission (PFS1) and administration of a salvage therapy.
Summary
One fourth of R/R PCNSL are asymptomatic underlining the need for systematic neuroimaging in surveillance. Duration of first remission (PFS1) is a strong prognostic factor. Salvage chemotherapy followed by consolidation with ICT+ASCT is associated with prolonged remission in a subset of patients.
Keyword(s): CNS lymphoma
Session topic: Optimization and innovation in treating aggressive lymphomas


