
Contributions
Type: Publication Only
Background
There is a spectrum of severity of haemophilia, defined as 'mild', 'moderate' or 'severe' according to the plasma levels of FVIII or FIX activity. Mild haemophilia may not be diagnosed until a minor surgery causes prolonged bleeding. Although general surgery in patients with 'mild' haemophilia has become more common, the surgical literature concerning these patiens remains limited.
Aims
The purpose of this single centre retrospective study was to investigate perioperative management and outcome of mild haemophiliac patients undergoing different surgical procedures.
Methods
For this study, we revised 12 mild hemophilia patients, who underwent 31 surgical procedures between 2008 and 2014 at our institution. Classification into minor/major surgery was carried out according to the BUPA system. We analized the hematologic diagnosis, type of surgery, genetic mutation linked to haemophilia, treatment undertaken to correct the bleeding disorders, the dose and duration of clotting factor administrated and post-surgical complications.
Results
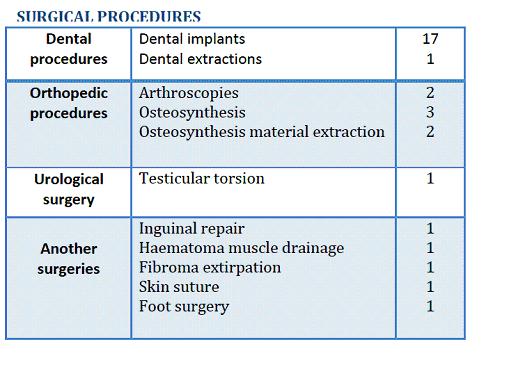
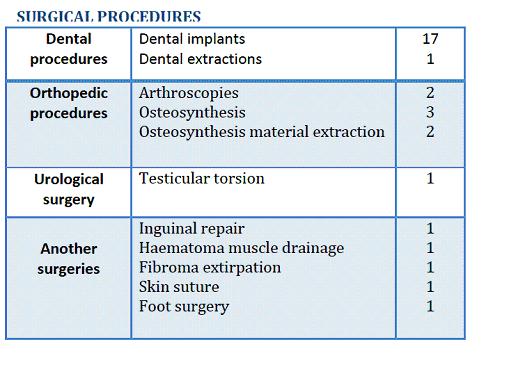
We revised a total of 31 surgical procedures performed in 12 mild haemophilia patients, 9 Haemophilia A (HA) and 3 Haemophilia B (HB). Median age at surgery 37 years (range: 20-54). No patients received an anticoagulatory prophilaxys for perioperative management. Among this haemophiliac group, 5 patients (41.6%) were hepatitis C seropositive who did not receive antiretroviral therapy. We didn´t found any seropositive for HIV or other viral disease. Molecular study was available in 7 patients (6 HA and 1 HB). 6 patients showed missense mutations: exon 14 (p.Arg698Trp), Exon 7 (p.Val 266Ala), Exon 2 (c.6374G>A), exon 12 (p.Arg593Cys), Exon25 (p.Asp2267Gly) and Exon 3 (p.Asp82Glu) and exon 2 (c.6374G>A) in 1 HB patient. Data about surgery, pre and post procedure treatment are seen in Table 1, 23 (74.2%) were minor and 8 (25.9%) were major surgery. Loco-regional anaesthesia was performed in 22 (70.9%) procedures. 8 (66.7%) patients (6 HA/2 HB) underwent more than one surgical procedure.
Pre and post-procedure dose of factor replacement treatment were adjusted according WFH guidelines. Plasma derived FVIII was employed in 2 patients during 4 procedures and recombinant FVIII or FIX were employed in 9 patients. Desmopressin alone and tranexamic acid alone were employed in 2 patients who underwent dental extraction (no wisdom tooth). Regarding minor procedures, 20 patients received Tranexamic Acid IV on postoperative days 1, 2 and 3. Before surgery, 1 patient who underwent 1 surgical procedure (dental extraction) showed a baseline factor level 5%>10%, 6 patients (12 procedures) showed factor levels 10%>20%, 5 patients levels 21%>30% (16 procedures) and 2 patients (2 procedures) 31%>40%. One HB patient (3.2% of all procedures) with a baseline factor level of 7.6% developed local bleeding after dental extraction although preoperative dose of recombinant FIX was administered, and he required one additional dose of recombinant FIX. No inhibitor development was observed.
Summary
Surgical procedures in patients with mild haemophilia can be performed with low hemorrhagic morbidity rates when there is good haematological support and appropriate hemostatic treatment. There was no association between the type of product used in perioperative period and inhibitor development in our group of patients. It is important that minor surgery should be scheduled to use desmopressin analogs +/- antifybrinolytics agents instead of recombinant clotting factor VIII/IX to minimize the risks of therapies and reduce overall treatment costs.
Keyword(s): Hemophilia, Recombinant factor, Surgery
Session topic: Publication Only
Type: Publication Only
Background
There is a spectrum of severity of haemophilia, defined as 'mild', 'moderate' or 'severe' according to the plasma levels of FVIII or FIX activity. Mild haemophilia may not be diagnosed until a minor surgery causes prolonged bleeding. Although general surgery in patients with 'mild' haemophilia has become more common, the surgical literature concerning these patiens remains limited.
Aims
The purpose of this single centre retrospective study was to investigate perioperative management and outcome of mild haemophiliac patients undergoing different surgical procedures.
Methods
For this study, we revised 12 mild hemophilia patients, who underwent 31 surgical procedures between 2008 and 2014 at our institution. Classification into minor/major surgery was carried out according to the BUPA system. We analized the hematologic diagnosis, type of surgery, genetic mutation linked to haemophilia, treatment undertaken to correct the bleeding disorders, the dose and duration of clotting factor administrated and post-surgical complications.
Results
We revised a total of 31 surgical procedures performed in 12 mild haemophilia patients, 9 Haemophilia A (HA) and 3 Haemophilia B (HB). Median age at surgery 37 years (range: 20-54). No patients received an anticoagulatory prophilaxys for perioperative management. Among this haemophiliac group, 5 patients (41.6%) were hepatitis C seropositive who did not receive antiretroviral therapy. We didn´t found any seropositive for HIV or other viral disease. Molecular study was available in 7 patients (6 HA and 1 HB). 6 patients showed missense mutations: exon 14 (p.Arg698Trp), Exon 7 (p.Val 266Ala), Exon 2 (c.6374G>A), exon 12 (p.Arg593Cys), Exon25 (p.Asp2267Gly) and Exon 3 (p.Asp82Glu) and exon 2 (c.6374G>A) in 1 HB patient. Data about surgery, pre and post procedure treatment are seen in Table 1, 23 (74.2%) were minor and 8 (25.9%) were major surgery. Loco-regional anaesthesia was performed in 22 (70.9%) procedures. 8 (66.7%) patients (6 HA/2 HB) underwent more than one surgical procedure.
Pre and post-procedure dose of factor replacement treatment were adjusted according WFH guidelines. Plasma derived FVIII was employed in 2 patients during 4 procedures and recombinant FVIII or FIX were employed in 9 patients. Desmopressin alone and tranexamic acid alone were employed in 2 patients who underwent dental extraction (no wisdom tooth). Regarding minor procedures, 20 patients received Tranexamic Acid IV on postoperative days 1, 2 and 3. Before surgery, 1 patient who underwent 1 surgical procedure (dental extraction) showed a baseline factor level 5%>10%, 6 patients (12 procedures) showed factor levels 10%>20%, 5 patients levels 21%>30% (16 procedures) and 2 patients (2 procedures) 31%>40%. One HB patient (3.2% of all procedures) with a baseline factor level of 7.6% developed local bleeding after dental extraction although preoperative dose of recombinant FIX was administered, and he required one additional dose of recombinant FIX. No inhibitor development was observed.
Summary
Surgical procedures in patients with mild haemophilia can be performed with low hemorrhagic morbidity rates when there is good haematological support and appropriate hemostatic treatment. There was no association between the type of product used in perioperative period and inhibitor development in our group of patients. It is important that minor surgery should be scheduled to use desmopressin analogs +/- antifybrinolytics agents instead of recombinant clotting factor VIII/IX to minimize the risks of therapies and reduce overall treatment costs.
Keyword(s): Hemophilia, Recombinant factor, Surgery
Session topic: Publication Only


