CLINICAL IMPACT OF EARLY RECOVERY OF POST-TRANSPLANT PERIPHERAL BLOOD ABSOLUTE LYMPHOCYTE COUNT ON THE OUTCOME OF FRONTLINE AUTOLOGOUS STEM CELL TRANSPLANTATION FOR DIFFUSE LARGE B-CELL LYMPHOMA
(Abstract release date: 05/21/15)
EHA Library. Kim Y. 06/12/15; 103040; PB1676
Disclosure(s): Yonsei University Severance hospitalInternal Medicine

Yundeok Kim
Contributions
Contributions
Abstract
Abstract: PB1676
Type: Publication Only
Background
Several studies have shown that lymphopenia, which is considered a surrogate marker of immunological incompetence, has considered as an adverse prognostic factor in Non-Hodgkin`s lymphoma (NHL). Recently, it has been suggested that early recovery of an absolute lymphocyte count (ALC) at 2-3 weeks following therapy has been associated with superior progression-free survival (PFS) and overall survival (OS) in patients who received autologous stem cell transplantation (ASCT) for NHL,. However, the prognostic significance of early recovery of peripheral ALC following frontline ASCT in diffuse large B-cell lymphoma (DLBCL) remains unclear.
Aims
The purpose of this study was to investigate the prognostic role of early recovery of peripheral ALC after ASCT in patients with DLBCL who underwent frontline ASCT.
Methods
We retrospectively evaluated 51 patients who underwent ASCT for DLBCL at Yonsei University Severance Hospital between January 2006 and 2014. All patients were treated with R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone) every 3 weeks for 3 to 8 cycles as first-line therapy and received frontline ASCT as consolidation. Most patients (n=40) received intravenous busulfan-based conditioning chemotherapy. The ALC at the time of D+14 after ASCT was obtained. Receiver operating characteristics (ROC) analysis was performed to determine the optimal cut-point for the ALC.
Results
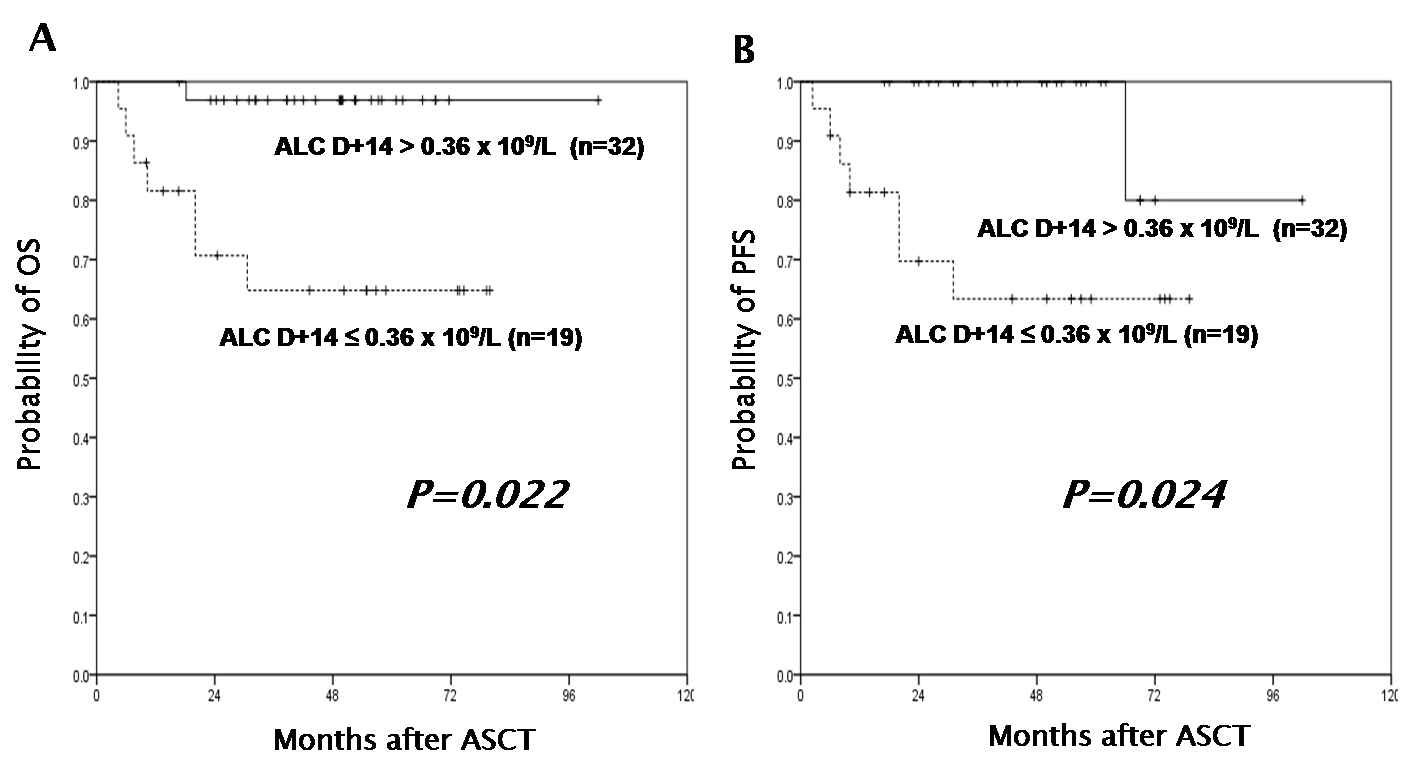
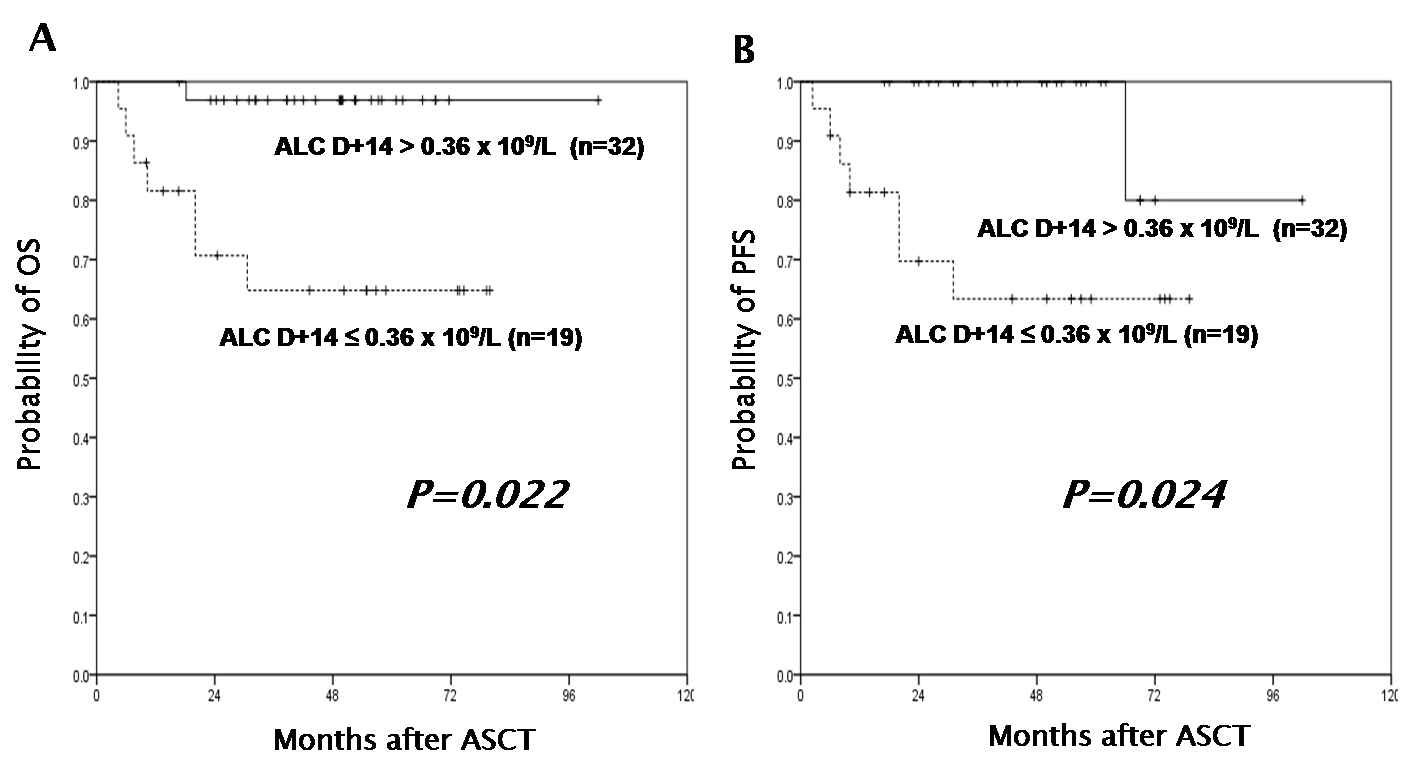
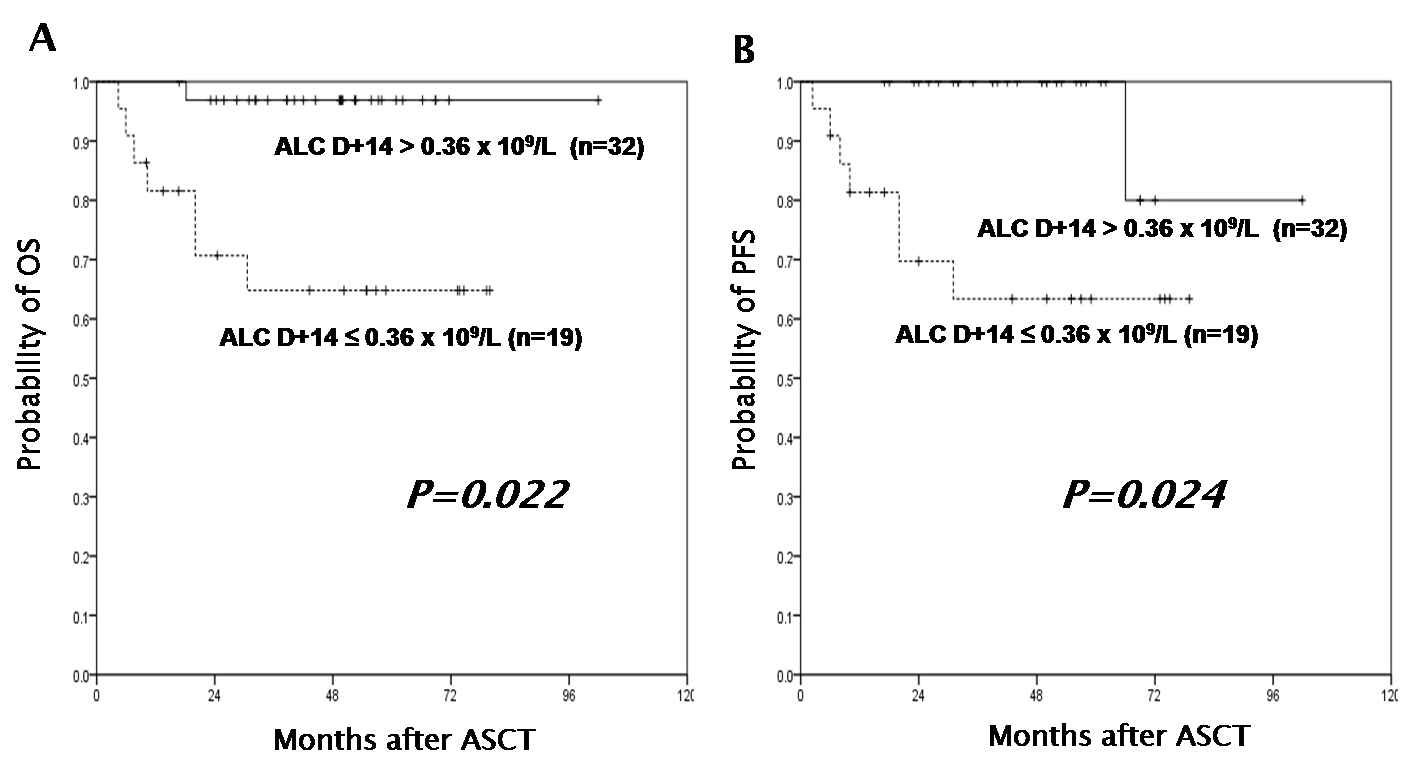
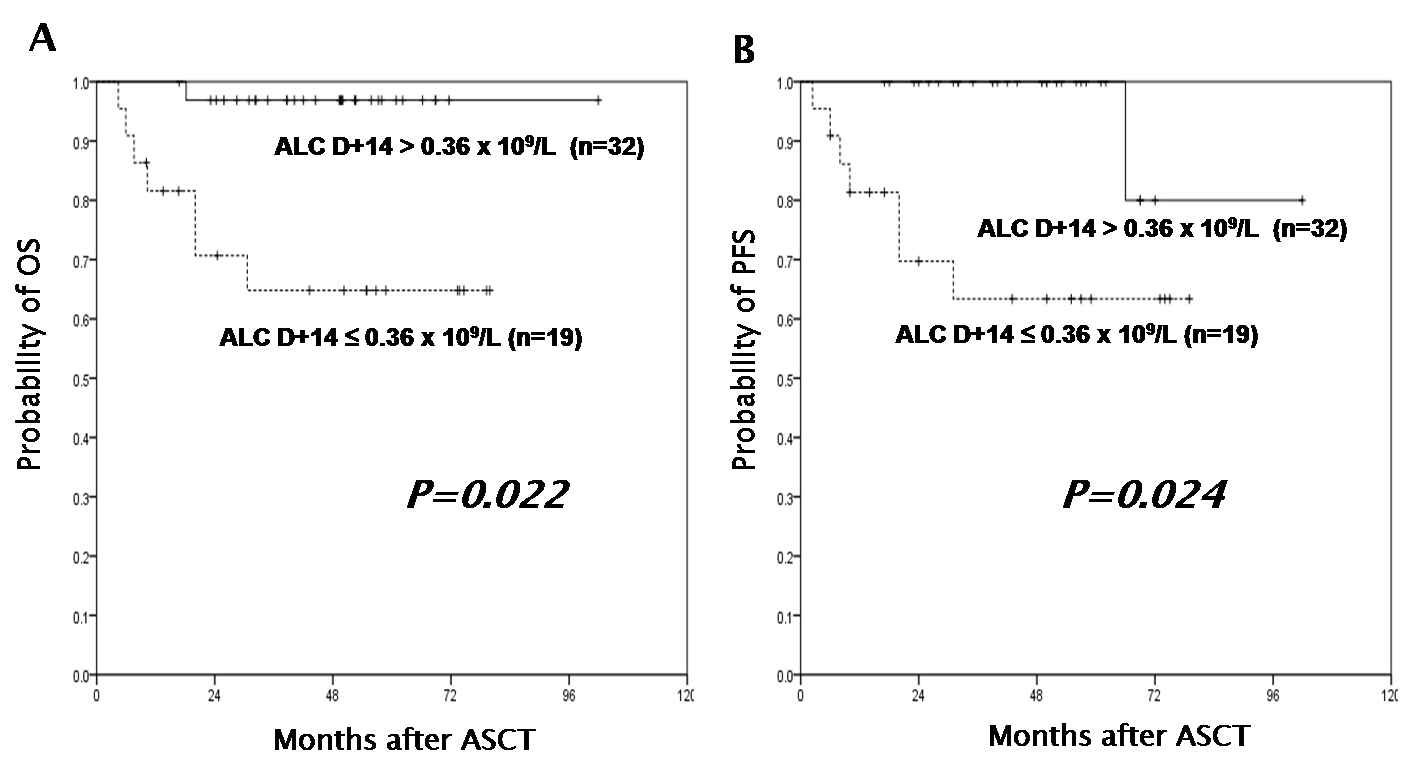
The study population included 51 patients with a median age of 53 years (range, 19-66 years). Fourty-six (90.2%) had stage IV disease according to the Ann Arbor staging system. Most patients (87.3%) were younger than 60 years. Thirty-five (68.8%) patients had B symptoms. International prognostic index (IPI) was low in 2 (4%), Low-intermediate in 15 (30%), high-intermediate in 25 (50%) and high in 8 (16%). Pre-transplant disease status was complete remission (CR) in 30 (58.8%) patients and partial remission (PR) in 21 (41.2%) patients. The median ALC at D+14 after ASCT was 0.43 x 109/L (range, 0.03-1.57 x 109/L). The ROC curve analysis identified 0.36 x 109/L as the cutoff value of ALC at D+14 for predicting relapse with an area under curve of 0,759 (95% CI, 0.628-0.890, P=0.020). When comparing the baseline clinical characteristics of patients with an ALC at D+14 of ≤ 0.36 x 109/L (low ALC group, n=19) and >0.36 x 109/L (high ALC group, n=32), no significant difference was found between two groups, except for a female dominance and presence of B symptoms at diagnosis in the low ALC group. The median survival of patients following ASCT was 49.4 months (range, 4.4-101.9 months). In a univariate analysis from the time of ASCT, it appears that high ALC at D+14 was associated with a better OS (HR=0.083; 95% CI 0.010-0.694, P=0.022) and PFS (HR=0.086; 95%CI 0.010-0.720, P=0.024) and event-free survival (EFS) (HR=0.283; 95% CI 0.082-0.971, P=0.045). Multivariate analysis revealed that high ALC at D+14 was a good prognostic factor for OS (HR=0.086; 95%CI 0.008-0.979, P=0.048).
Summary
The early recovery of ALC at D+14 after ASCT can be regarded as a good prognostic marker in patients with DLBCL who underwent frontline ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL, Lymphocyte
Session topic: Publication Only
Type: Publication Only
Background
Several studies have shown that lymphopenia, which is considered a surrogate marker of immunological incompetence, has considered as an adverse prognostic factor in Non-Hodgkin`s lymphoma (NHL). Recently, it has been suggested that early recovery of an absolute lymphocyte count (ALC) at 2-3 weeks following therapy has been associated with superior progression-free survival (PFS) and overall survival (OS) in patients who received autologous stem cell transplantation (ASCT) for NHL,. However, the prognostic significance of early recovery of peripheral ALC following frontline ASCT in diffuse large B-cell lymphoma (DLBCL) remains unclear.
Aims
The purpose of this study was to investigate the prognostic role of early recovery of peripheral ALC after ASCT in patients with DLBCL who underwent frontline ASCT.
Methods
We retrospectively evaluated 51 patients who underwent ASCT for DLBCL at Yonsei University Severance Hospital between January 2006 and 2014. All patients were treated with R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone) every 3 weeks for 3 to 8 cycles as first-line therapy and received frontline ASCT as consolidation. Most patients (n=40) received intravenous busulfan-based conditioning chemotherapy. The ALC at the time of D+14 after ASCT was obtained. Receiver operating characteristics (ROC) analysis was performed to determine the optimal cut-point for the ALC.
Results
The study population included 51 patients with a median age of 53 years (range, 19-66 years). Fourty-six (90.2%) had stage IV disease according to the Ann Arbor staging system. Most patients (87.3%) were younger than 60 years. Thirty-five (68.8%) patients had B symptoms. International prognostic index (IPI) was low in 2 (4%), Low-intermediate in 15 (30%), high-intermediate in 25 (50%) and high in 8 (16%). Pre-transplant disease status was complete remission (CR) in 30 (58.8%) patients and partial remission (PR) in 21 (41.2%) patients. The median ALC at D+14 after ASCT was 0.43 x 109/L (range, 0.03-1.57 x 109/L). The ROC curve analysis identified 0.36 x 109/L as the cutoff value of ALC at D+14 for predicting relapse with an area under curve of 0,759 (95% CI, 0.628-0.890, P=0.020). When comparing the baseline clinical characteristics of patients with an ALC at D+14 of ≤ 0.36 x 109/L (low ALC group, n=19) and >0.36 x 109/L (high ALC group, n=32), no significant difference was found between two groups, except for a female dominance and presence of B symptoms at diagnosis in the low ALC group. The median survival of patients following ASCT was 49.4 months (range, 4.4-101.9 months). In a univariate analysis from the time of ASCT, it appears that high ALC at D+14 was associated with a better OS (HR=0.083; 95% CI 0.010-0.694, P=0.022) and PFS (HR=0.086; 95%CI 0.010-0.720, P=0.024) and event-free survival (EFS) (HR=0.283; 95% CI 0.082-0.971, P=0.045). Multivariate analysis revealed that high ALC at D+14 was a good prognostic factor for OS (HR=0.086; 95%CI 0.008-0.979, P=0.048).
Summary
The early recovery of ALC at D+14 after ASCT can be regarded as a good prognostic marker in patients with DLBCL who underwent frontline ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL, Lymphocyte
Session topic: Publication Only
Abstract: PB1676
Type: Publication Only
Background
Several studies have shown that lymphopenia, which is considered a surrogate marker of immunological incompetence, has considered as an adverse prognostic factor in Non-Hodgkin`s lymphoma (NHL). Recently, it has been suggested that early recovery of an absolute lymphocyte count (ALC) at 2-3 weeks following therapy has been associated with superior progression-free survival (PFS) and overall survival (OS) in patients who received autologous stem cell transplantation (ASCT) for NHL,. However, the prognostic significance of early recovery of peripheral ALC following frontline ASCT in diffuse large B-cell lymphoma (DLBCL) remains unclear.
Aims
The purpose of this study was to investigate the prognostic role of early recovery of peripheral ALC after ASCT in patients with DLBCL who underwent frontline ASCT.
Methods
We retrospectively evaluated 51 patients who underwent ASCT for DLBCL at Yonsei University Severance Hospital between January 2006 and 2014. All patients were treated with R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone) every 3 weeks for 3 to 8 cycles as first-line therapy and received frontline ASCT as consolidation. Most patients (n=40) received intravenous busulfan-based conditioning chemotherapy. The ALC at the time of D+14 after ASCT was obtained. Receiver operating characteristics (ROC) analysis was performed to determine the optimal cut-point for the ALC.
Results
The study population included 51 patients with a median age of 53 years (range, 19-66 years). Fourty-six (90.2%) had stage IV disease according to the Ann Arbor staging system. Most patients (87.3%) were younger than 60 years. Thirty-five (68.8%) patients had B symptoms. International prognostic index (IPI) was low in 2 (4%), Low-intermediate in 15 (30%), high-intermediate in 25 (50%) and high in 8 (16%). Pre-transplant disease status was complete remission (CR) in 30 (58.8%) patients and partial remission (PR) in 21 (41.2%) patients. The median ALC at D+14 after ASCT was 0.43 x 109/L (range, 0.03-1.57 x 109/L). The ROC curve analysis identified 0.36 x 109/L as the cutoff value of ALC at D+14 for predicting relapse with an area under curve of 0,759 (95% CI, 0.628-0.890, P=0.020). When comparing the baseline clinical characteristics of patients with an ALC at D+14 of ≤ 0.36 x 109/L (low ALC group, n=19) and >0.36 x 109/L (high ALC group, n=32), no significant difference was found between two groups, except for a female dominance and presence of B symptoms at diagnosis in the low ALC group. The median survival of patients following ASCT was 49.4 months (range, 4.4-101.9 months). In a univariate analysis from the time of ASCT, it appears that high ALC at D+14 was associated with a better OS (HR=0.083; 95% CI 0.010-0.694, P=0.022) and PFS (HR=0.086; 95%CI 0.010-0.720, P=0.024) and event-free survival (EFS) (HR=0.283; 95% CI 0.082-0.971, P=0.045). Multivariate analysis revealed that high ALC at D+14 was a good prognostic factor for OS (HR=0.086; 95%CI 0.008-0.979, P=0.048).
Summary
The early recovery of ALC at D+14 after ASCT can be regarded as a good prognostic marker in patients with DLBCL who underwent frontline ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL, Lymphocyte
Session topic: Publication Only
Type: Publication Only
Background
Several studies have shown that lymphopenia, which is considered a surrogate marker of immunological incompetence, has considered as an adverse prognostic factor in Non-Hodgkin`s lymphoma (NHL). Recently, it has been suggested that early recovery of an absolute lymphocyte count (ALC) at 2-3 weeks following therapy has been associated with superior progression-free survival (PFS) and overall survival (OS) in patients who received autologous stem cell transplantation (ASCT) for NHL,. However, the prognostic significance of early recovery of peripheral ALC following frontline ASCT in diffuse large B-cell lymphoma (DLBCL) remains unclear.
Aims
The purpose of this study was to investigate the prognostic role of early recovery of peripheral ALC after ASCT in patients with DLBCL who underwent frontline ASCT.
Methods
We retrospectively evaluated 51 patients who underwent ASCT for DLBCL at Yonsei University Severance Hospital between January 2006 and 2014. All patients were treated with R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone) every 3 weeks for 3 to 8 cycles as first-line therapy and received frontline ASCT as consolidation. Most patients (n=40) received intravenous busulfan-based conditioning chemotherapy. The ALC at the time of D+14 after ASCT was obtained. Receiver operating characteristics (ROC) analysis was performed to determine the optimal cut-point for the ALC.
Results
The study population included 51 patients with a median age of 53 years (range, 19-66 years). Fourty-six (90.2%) had stage IV disease according to the Ann Arbor staging system. Most patients (87.3%) were younger than 60 years. Thirty-five (68.8%) patients had B symptoms. International prognostic index (IPI) was low in 2 (4%), Low-intermediate in 15 (30%), high-intermediate in 25 (50%) and high in 8 (16%). Pre-transplant disease status was complete remission (CR) in 30 (58.8%) patients and partial remission (PR) in 21 (41.2%) patients. The median ALC at D+14 after ASCT was 0.43 x 109/L (range, 0.03-1.57 x 109/L). The ROC curve analysis identified 0.36 x 109/L as the cutoff value of ALC at D+14 for predicting relapse with an area under curve of 0,759 (95% CI, 0.628-0.890, P=0.020). When comparing the baseline clinical characteristics of patients with an ALC at D+14 of ≤ 0.36 x 109/L (low ALC group, n=19) and >0.36 x 109/L (high ALC group, n=32), no significant difference was found between two groups, except for a female dominance and presence of B symptoms at diagnosis in the low ALC group. The median survival of patients following ASCT was 49.4 months (range, 4.4-101.9 months). In a univariate analysis from the time of ASCT, it appears that high ALC at D+14 was associated with a better OS (HR=0.083; 95% CI 0.010-0.694, P=0.022) and PFS (HR=0.086; 95%CI 0.010-0.720, P=0.024) and event-free survival (EFS) (HR=0.283; 95% CI 0.082-0.971, P=0.045). Multivariate analysis revealed that high ALC at D+14 was a good prognostic factor for OS (HR=0.086; 95%CI 0.008-0.979, P=0.048).
Summary
The early recovery of ALC at D+14 after ASCT can be regarded as a good prognostic marker in patients with DLBCL who underwent frontline ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL, Lymphocyte
Session topic: Publication Only
{{ help_message }}
{{filter}}


