high dose chemotherapy of paraproteinemic hemoblastosis

Contributions
Type: Publication Only
Background
Patients (pts) with multiple myeloma (MM) face an high risk of thrombosis. We are talking about pts-related, disease-related and therapy-related risk factors. Meanwhile no specific scale exists to assess the risk of thrombotic complications for MM pts. We suppose that the Caprini scale is the most comprehensive instrument for validation of individual risk factors and it can be used not only for surgery pts.
Aims
The study was aimed to investigate the blood coagulation status in MM pts depending on the individual risk assessment on the Caprini scale before and during peripheral blood stem cell (PBSC) mobilization.
Methods
The study’s sample consisted of 30 pts - candidates for high dose chemotherapy. There were 19 males and 11 females at the age of 27 – 64 years (median 55). After bortezomib-containig induction therapy 7 of them achieved PR, 16 – VGPR and 7 – CR.
PBSC mobilization was performed by using cyclophosphamide (CY, 4g/m2) and granulocyte colony-stimulating factor (G-CSF, 5mcg/kg/day).
According to the internal protocol all pts had prevention heparin-sulphate continuous infusion (in initial dose 500 IU/hour), starting the day before CY introduction and stopping the next day after finish last PBSC collection.
All pts were assessed with Caprini model.
Hemostasis analysis was performed 5 times and included validation the results of activated partial thromboplasin time (APTT, 25 – 38 sec) and concentration of D-dimer (0 – 500 mkg/l). Hypercoagulation was considered in cases when APTT < 25 sec and D-dimer > 500 mkg/l. And hypocoagulation was estimated by data APTT > 38 sec.
Statistical analysis was performed with SAS 9.1 (using the GLM procedure).
Results
This group of pts had 3 - 6 (mean 4,4 ± 0,96) scores on the Caprini scale. Initially (before heparin administration) APTT evaluation showed normal coagulation in 26 pts and hypocoagulation in 4 pts (mean 34 sec; 95% CI 32 – 36 sec). D-dimer was normal in 25 pts and increased in 4 cases (mean 309,8 mkg/l; 95% CI 170,0– 449,5 mkg/l).
APTT had significantly (p < 0,05) changed to hypocoagulability on the next day after starting thromboprophylaxis and in a state of agranulocytosis became 39 sec (95% CI 36 – 46 sec) and 40 sec (95% CI 36 – 50 sec) respectively. On the next day after CY infusion, APTT was statistically significantly decreased (p < 0,05) reaching 34 sec (95% CI 32 – 37 sec). On the day of PBSC collection the mean APTT was 38 sec (95% CI 37 – 43 sec).
Concentration of D-dimer was not modified in response to heparin or CY infusion or in a state of agranulocytosis and it icreased (p < 0,05) reaching 476 mkg/l (95% CI 326 - 626 mkg/l) on the day of PBSC collection.
Thrombotic complications were detected in 2 pts from a very high risk group (> 5 score) on the Caprini scale.
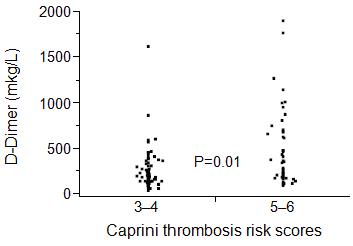
The analysis of our results showed statistically significant increase of (p = 0,01) concentration of D-dimer in pts with the score of 5 or 6 compared pts with the score of 3 or 4 score (figure 1).
Pts in CR demonstrated no significant difference in coagulation status compared to pts in VGPR or PR.
Summary
The possibility to use the Carpini scale to assess an individual risk of thrombotic complications for patients with MM has been confirmed clinically and by results of laboratory tests.
Keyword(s): D-dimer, Mobilization, Multiple myeloma, Thrombosis
Session topic: Publication Only
Type: Publication Only
Background
Patients (pts) with multiple myeloma (MM) face an high risk of thrombosis. We are talking about pts-related, disease-related and therapy-related risk factors. Meanwhile no specific scale exists to assess the risk of thrombotic complications for MM pts. We suppose that the Caprini scale is the most comprehensive instrument for validation of individual risk factors and it can be used not only for surgery pts.
Aims
The study was aimed to investigate the blood coagulation status in MM pts depending on the individual risk assessment on the Caprini scale before and during peripheral blood stem cell (PBSC) mobilization.
Methods
The study’s sample consisted of 30 pts - candidates for high dose chemotherapy. There were 19 males and 11 females at the age of 27 – 64 years (median 55). After bortezomib-containig induction therapy 7 of them achieved PR, 16 – VGPR and 7 – CR.
PBSC mobilization was performed by using cyclophosphamide (CY, 4g/m2) and granulocyte colony-stimulating factor (G-CSF, 5mcg/kg/day).
According to the internal protocol all pts had prevention heparin-sulphate continuous infusion (in initial dose 500 IU/hour), starting the day before CY introduction and stopping the next day after finish last PBSC collection.
All pts were assessed with Caprini model.
Hemostasis analysis was performed 5 times and included validation the results of activated partial thromboplasin time (APTT, 25 – 38 sec) and concentration of D-dimer (0 – 500 mkg/l). Hypercoagulation was considered in cases when APTT < 25 sec and D-dimer > 500 mkg/l. And hypocoagulation was estimated by data APTT > 38 sec.
Statistical analysis was performed with SAS 9.1 (using the GLM procedure).
Results
This group of pts had 3 - 6 (mean 4,4 ± 0,96) scores on the Caprini scale. Initially (before heparin administration) APTT evaluation showed normal coagulation in 26 pts and hypocoagulation in 4 pts (mean 34 sec; 95% CI 32 – 36 sec). D-dimer was normal in 25 pts and increased in 4 cases (mean 309,8 mkg/l; 95% CI 170,0– 449,5 mkg/l).
APTT had significantly (p < 0,05) changed to hypocoagulability on the next day after starting thromboprophylaxis and in a state of agranulocytosis became 39 sec (95% CI 36 – 46 sec) and 40 sec (95% CI 36 – 50 sec) respectively. On the next day after CY infusion, APTT was statistically significantly decreased (p < 0,05) reaching 34 sec (95% CI 32 – 37 sec). On the day of PBSC collection the mean APTT was 38 sec (95% CI 37 – 43 sec).
Concentration of D-dimer was not modified in response to heparin or CY infusion or in a state of agranulocytosis and it icreased (p < 0,05) reaching 476 mkg/l (95% CI 326 - 626 mkg/l) on the day of PBSC collection.
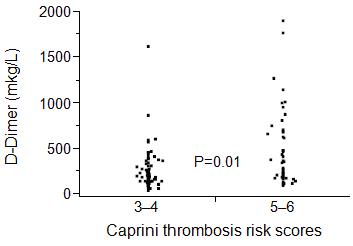
Thrombotic complications were detected in 2 pts from a very high risk group (> 5 score) on the Caprini scale.
The analysis of our results showed statistically significant increase of (p = 0,01) concentration of D-dimer in pts with the score of 5 or 6 compared pts with the score of 3 or 4 score (figure 1).
Pts in CR demonstrated no significant difference in coagulation status compared to pts in VGPR or PR.
Summary
The possibility to use the Carpini scale to assess an individual risk of thrombotic complications for patients with MM has been confirmed clinically and by results of laboratory tests.
Keyword(s): D-dimer, Mobilization, Multiple myeloma, Thrombosis
Session topic: Publication Only


