Lymphoma center

Contributions
Type: Publication Only
Background
Most of data about the clinical outcome of patients with chronic lymphocytic leukemia (CLL) come from patients participating in clinical trials. Such trials typically have strict eligibility criteria based on performance status and organ function. Little is known about the organ function of unselected patients (i.e., regardless of whether they are eligible for trials). Adult comorbidity evaluation-27 (ACE-27), Cumulative Illness Rating Scale (CIRS) and hematopoietic cell transplantation comorbidity index (HCT-CI) are comorbidity indexes that take concurrent presence of nonmalignant diseases into account when explaining survival. They differ in both the number and categorization of comorbidities.
Aims
We investigated the prognostic significance of three comorbidity indexes in adition to standard prognostic tools in a sample of 74 patients with CLL.
Methods
We retrospectively evaluated the impact of ACE-27, CIRS and HCT-CI in a cohort of 74 adult patients with chronic lymphocytic leukemia (HLL) treated with Fludarabine-Cyclophosphamide combination. Also we tested impact of standard prognostic tool available in daily practice as age, gender, Rai/Binet clinical stage, LDH level, type of bone marrow infiltration and CD38 expression. Patient and survival data were acquired from inpatient hospital records. Cox hazard regression model was used to analyze overall survival according to standard prognostic factors and comorbidities classified by the ACE-27, CIRS and HCT-CI.
Results
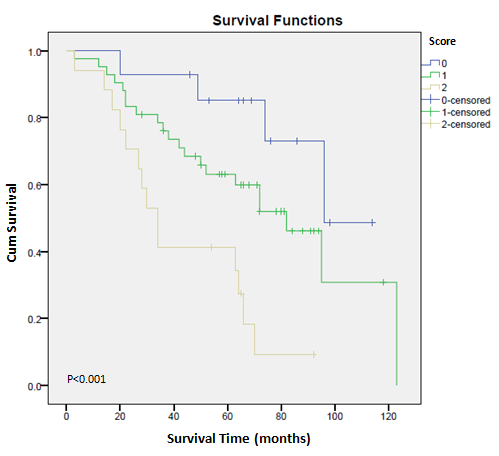
Median follow up of our group was was 5 years (60 months) while median overall and progression free survival was 72 and 32.5 months, respectively. We found a significant association between CIRS and bone marrow infiltration pattern and overall survival (p=0.037; RR=2.0; 95%CI for RR 1.1-4.0 for CIRS>15 and p=0.014; RR=2.3; 95%CI for RR 1.2-4.5 for diffuse type of bone marrow infiltration). Other two comorbidity indexes – ACE-27 and HCT-CI and standard prognostic factors did not outperform the survival model, while in multivariate analysis CIRS>15 and diffuse type of marrow infiltration remained the most important predictors of overall survival (p=0,009 and p=0,004, respectively). We developed a new scoring system based on the CIRS score value and bone marrow infiltration pattern. Patients with CIRS≤15 and without diffuse type of marrow infiltration were of low risk (score 0), patients with CIRS>15 or diffuse bone marrow infiltration pattern corresponded with intermediate risk (score 1), while patients with both CIRS>15 and diffuse type of bone marrow infiltration represented high risk group (score 2). Median overall survival for patients with score 0, 1 and 2 was 96, 82 and 34 months, respectively, which makes this new score a good predictor of mortality among patients with chronic lymphocytic leukemia (p<0.001; RR=2.6; 95%CI for RR 1.5-4.5).
Summary
In our group of adult CLL patients the overall survival is associated with the presence of comorbidities defined by the CIRS index. CIRS and type of bone marrow infiltration present a superior comorbidity risk-adjustment model for CLL survival prediction.
Keyword(s): Chronic lymphocytic leukemia, Comorbidities
Session topic: Publication Only
Type: Publication Only
Background
Most of data about the clinical outcome of patients with chronic lymphocytic leukemia (CLL) come from patients participating in clinical trials. Such trials typically have strict eligibility criteria based on performance status and organ function. Little is known about the organ function of unselected patients (i.e., regardless of whether they are eligible for trials). Adult comorbidity evaluation-27 (ACE-27), Cumulative Illness Rating Scale (CIRS) and hematopoietic cell transplantation comorbidity index (HCT-CI) are comorbidity indexes that take concurrent presence of nonmalignant diseases into account when explaining survival. They differ in both the number and categorization of comorbidities.
Aims
We investigated the prognostic significance of three comorbidity indexes in adition to standard prognostic tools in a sample of 74 patients with CLL.
Methods
We retrospectively evaluated the impact of ACE-27, CIRS and HCT-CI in a cohort of 74 adult patients with chronic lymphocytic leukemia (HLL) treated with Fludarabine-Cyclophosphamide combination. Also we tested impact of standard prognostic tool available in daily practice as age, gender, Rai/Binet clinical stage, LDH level, type of bone marrow infiltration and CD38 expression. Patient and survival data were acquired from inpatient hospital records. Cox hazard regression model was used to analyze overall survival according to standard prognostic factors and comorbidities classified by the ACE-27, CIRS and HCT-CI.
Results
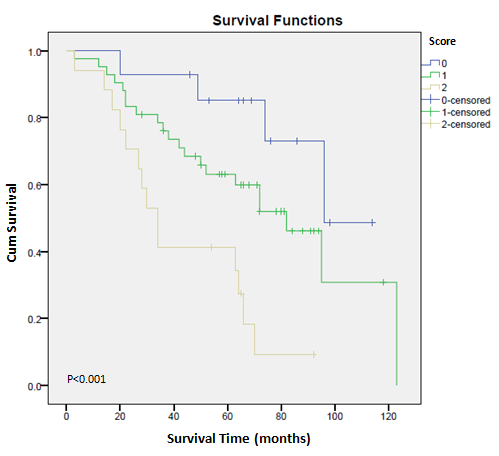
Median follow up of our group was was 5 years (60 months) while median overall and progression free survival was 72 and 32.5 months, respectively. We found a significant association between CIRS and bone marrow infiltration pattern and overall survival (p=0.037; RR=2.0; 95%CI for RR 1.1-4.0 for CIRS>15 and p=0.014; RR=2.3; 95%CI for RR 1.2-4.5 for diffuse type of bone marrow infiltration). Other two comorbidity indexes – ACE-27 and HCT-CI and standard prognostic factors did not outperform the survival model, while in multivariate analysis CIRS>15 and diffuse type of marrow infiltration remained the most important predictors of overall survival (p=0,009 and p=0,004, respectively). We developed a new scoring system based on the CIRS score value and bone marrow infiltration pattern. Patients with CIRS≤15 and without diffuse type of marrow infiltration were of low risk (score 0), patients with CIRS>15 or diffuse bone marrow infiltration pattern corresponded with intermediate risk (score 1), while patients with both CIRS>15 and diffuse type of bone marrow infiltration represented high risk group (score 2). Median overall survival for patients with score 0, 1 and 2 was 96, 82 and 34 months, respectively, which makes this new score a good predictor of mortality among patients with chronic lymphocytic leukemia (p<0.001; RR=2.6; 95%CI for RR 1.5-4.5).
Summary
In our group of adult CLL patients the overall survival is associated with the presence of comorbidities defined by the CIRS index. CIRS and type of bone marrow infiltration present a superior comorbidity risk-adjustment model for CLL survival prediction.
Keyword(s): Chronic lymphocytic leukemia, Comorbidities
Session topic: Publication Only


