UPFRONT AUTOLOGOUS STEM CELL TRANSPLANTATION OVERCOMES A NEGATIVE IMPACT OF MALE GENDER IN HIGH-RISK DIFFUSE LARGE B-CELL LYMPHOMA PATIENTS TREATED WITH R-CHOP
(Abstract release date: 05/21/15)
EHA Library. Cho H. 06/12/15; 102985; PB1668
Disclosure(s): Severance Hospital
Dr. Hyunsoo Cho
Contributions
Contributions
Abstract
Abstract: PB1668
Type: Publication Only
Background
Combining rituximab to combination chemotherapy (R-CHOP) has significantly improved overall survival (OS) of patients with diffuse large B-cell lymphoma (DLBCL), but high-risk patients stratified according to the international prognostic index (IPI), non-germinal center B cells (non-GCB) subtype, and male patients have shown inferior treatment outcomes. Although the first-line treatment of patients with DLBCL is R-CHOP irrespective of the risk-group, there have been few studies evaluating the role of upfront ASCT as consolidative treatment strategy for high-risk DLBCL patients.
Aims
To investigate the role of upfront ASCT as consolidation after R-CHOP chemotherapy according to the gender in newly diagnosed advanced stage DLBCL patients.
Methods
We performed a multicenter retrospective analysis of 204 newly diagnosed DLBCL patients between January 2008 and December 2013. Patients who were younger than 65 years of age with advanced stage (Ann Arbor stage III or IV) and elevated serum lactate dehydrogenase were included. All the patients completed 4 to 8 cycles of planned R-CHOP chemotherapy and achieved at least PR after completion of planned R-CHOP chemotherapy.
Results
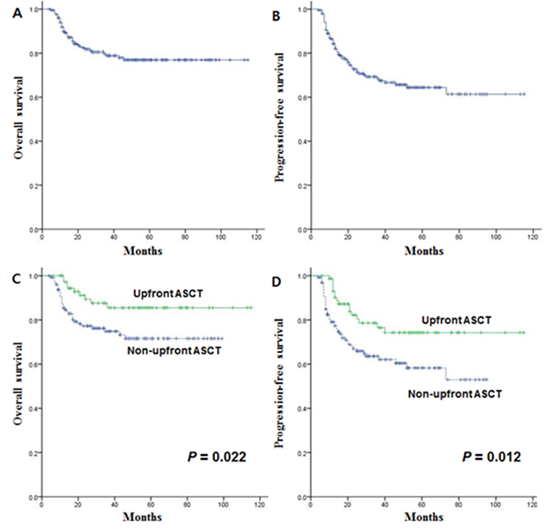
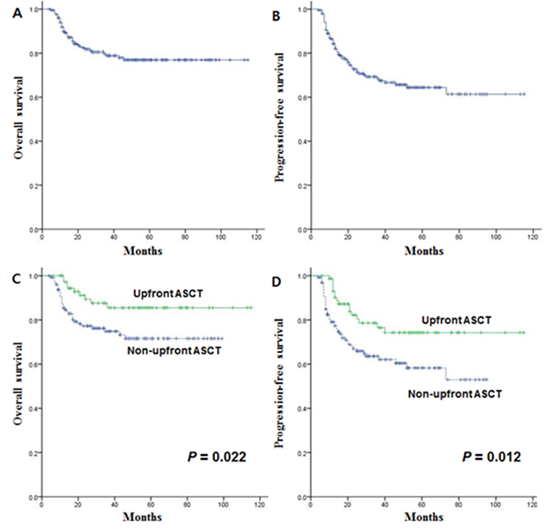
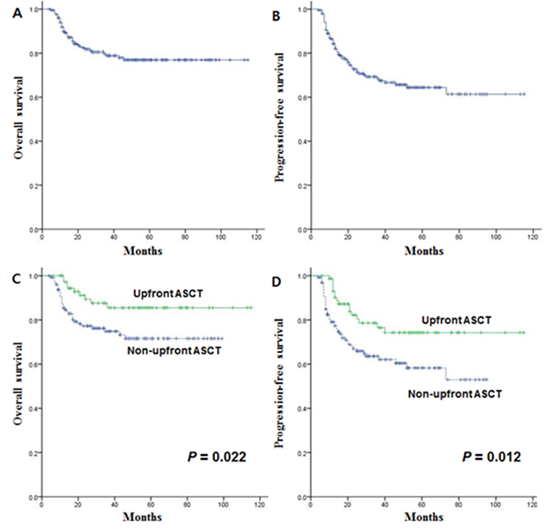
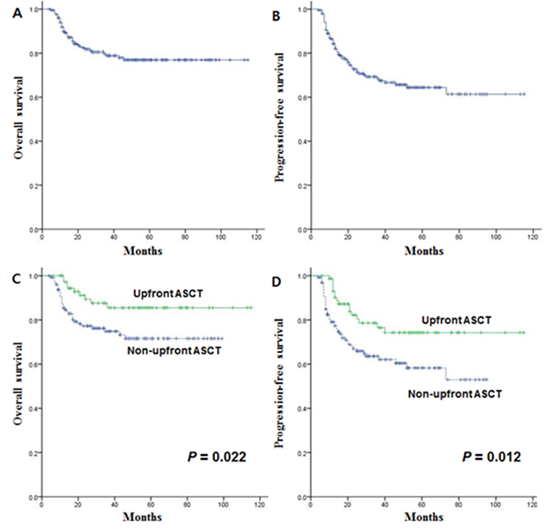
The median age at diagnosis was 50 (range 22-64) years and 111 (54.4%) patients were male. Median follow-up for surviving patients was 42 (range 4-115) months. Seventy-five (36.8%) patients underwent upfront ASCT as consolidation. Fifteen (11.6%) patients in the non-ASCT group (n=129) underwent ASCT after relapse. The 3-year OS and PFS rate for all patients were 78.8% and 68.4%, respectively. In multivariate analysis, non-CR after R-CHOP chemotherapy and non-upfront ASCT was associated with shorter OS (hazard ratio (HR) 2.57; 95% CI 1.34-4.95; P=0.005 and HR 2.97; 95% CI 1.38-6.40; P=0.005, respectively). Non-ASCT was also associated with shorter PFS in multivariate analysis (HR 2.26; 95% CI 1.25-4.07; P=0.014). Among the male patients, upfront ASCT showed superior OS and PFS compared to the non-ASCT group (P=0.016 and P=0.024, respectively). GCB subtype compared to the non-GCB subtype showed better PFS in male patients (P=0.026), but there were no difference in OS and PFS in male patients who received upfront ASCT. In female patients, non-CR after completion of chemotherapy was associated with shorter OS on multivariate analysis (P=0.024). However, survival differences in OS and PFS according to the disease status after the completion of chemotherapy were not observed in female patients who received upfront ASCT.
Summary
Upfront ASCT as consolidation after R-CHOP chemotherapy overcomes a negative impact of male gender and non-GCB subtype in male patients with high-risk DLBCL. Among female patients with high risk DLBCL, upfront ASCT after R-CHOP chemotherapy may overcome a negative impact of non-CR response to initial therapy. Additional data comparing with new regimens such as additional use of rituximab are necessary to find out the exact role of upfront ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL
Session topic: Publication Only
Type: Publication Only
Background
Combining rituximab to combination chemotherapy (R-CHOP) has significantly improved overall survival (OS) of patients with diffuse large B-cell lymphoma (DLBCL), but high-risk patients stratified according to the international prognostic index (IPI), non-germinal center B cells (non-GCB) subtype, and male patients have shown inferior treatment outcomes. Although the first-line treatment of patients with DLBCL is R-CHOP irrespective of the risk-group, there have been few studies evaluating the role of upfront ASCT as consolidative treatment strategy for high-risk DLBCL patients.
Aims
To investigate the role of upfront ASCT as consolidation after R-CHOP chemotherapy according to the gender in newly diagnosed advanced stage DLBCL patients.
Methods
We performed a multicenter retrospective analysis of 204 newly diagnosed DLBCL patients between January 2008 and December 2013. Patients who were younger than 65 years of age with advanced stage (Ann Arbor stage III or IV) and elevated serum lactate dehydrogenase were included. All the patients completed 4 to 8 cycles of planned R-CHOP chemotherapy and achieved at least PR after completion of planned R-CHOP chemotherapy.
Results
The median age at diagnosis was 50 (range 22-64) years and 111 (54.4%) patients were male. Median follow-up for surviving patients was 42 (range 4-115) months. Seventy-five (36.8%) patients underwent upfront ASCT as consolidation. Fifteen (11.6%) patients in the non-ASCT group (n=129) underwent ASCT after relapse. The 3-year OS and PFS rate for all patients were 78.8% and 68.4%, respectively. In multivariate analysis, non-CR after R-CHOP chemotherapy and non-upfront ASCT was associated with shorter OS (hazard ratio (HR) 2.57; 95% CI 1.34-4.95; P=0.005 and HR 2.97; 95% CI 1.38-6.40; P=0.005, respectively). Non-ASCT was also associated with shorter PFS in multivariate analysis (HR 2.26; 95% CI 1.25-4.07; P=0.014). Among the male patients, upfront ASCT showed superior OS and PFS compared to the non-ASCT group (P=0.016 and P=0.024, respectively). GCB subtype compared to the non-GCB subtype showed better PFS in male patients (P=0.026), but there were no difference in OS and PFS in male patients who received upfront ASCT. In female patients, non-CR after completion of chemotherapy was associated with shorter OS on multivariate analysis (P=0.024). However, survival differences in OS and PFS according to the disease status after the completion of chemotherapy were not observed in female patients who received upfront ASCT.
Summary
Upfront ASCT as consolidation after R-CHOP chemotherapy overcomes a negative impact of male gender and non-GCB subtype in male patients with high-risk DLBCL. Among female patients with high risk DLBCL, upfront ASCT after R-CHOP chemotherapy may overcome a negative impact of non-CR response to initial therapy. Additional data comparing with new regimens such as additional use of rituximab are necessary to find out the exact role of upfront ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL
Session topic: Publication Only
Abstract: PB1668
Type: Publication Only
Background
Combining rituximab to combination chemotherapy (R-CHOP) has significantly improved overall survival (OS) of patients with diffuse large B-cell lymphoma (DLBCL), but high-risk patients stratified according to the international prognostic index (IPI), non-germinal center B cells (non-GCB) subtype, and male patients have shown inferior treatment outcomes. Although the first-line treatment of patients with DLBCL is R-CHOP irrespective of the risk-group, there have been few studies evaluating the role of upfront ASCT as consolidative treatment strategy for high-risk DLBCL patients.
Aims
To investigate the role of upfront ASCT as consolidation after R-CHOP chemotherapy according to the gender in newly diagnosed advanced stage DLBCL patients.
Methods
We performed a multicenter retrospective analysis of 204 newly diagnosed DLBCL patients between January 2008 and December 2013. Patients who were younger than 65 years of age with advanced stage (Ann Arbor stage III or IV) and elevated serum lactate dehydrogenase were included. All the patients completed 4 to 8 cycles of planned R-CHOP chemotherapy and achieved at least PR after completion of planned R-CHOP chemotherapy.
Results
The median age at diagnosis was 50 (range 22-64) years and 111 (54.4%) patients were male. Median follow-up for surviving patients was 42 (range 4-115) months. Seventy-five (36.8%) patients underwent upfront ASCT as consolidation. Fifteen (11.6%) patients in the non-ASCT group (n=129) underwent ASCT after relapse. The 3-year OS and PFS rate for all patients were 78.8% and 68.4%, respectively. In multivariate analysis, non-CR after R-CHOP chemotherapy and non-upfront ASCT was associated with shorter OS (hazard ratio (HR) 2.57; 95% CI 1.34-4.95; P=0.005 and HR 2.97; 95% CI 1.38-6.40; P=0.005, respectively). Non-ASCT was also associated with shorter PFS in multivariate analysis (HR 2.26; 95% CI 1.25-4.07; P=0.014). Among the male patients, upfront ASCT showed superior OS and PFS compared to the non-ASCT group (P=0.016 and P=0.024, respectively). GCB subtype compared to the non-GCB subtype showed better PFS in male patients (P=0.026), but there were no difference in OS and PFS in male patients who received upfront ASCT. In female patients, non-CR after completion of chemotherapy was associated with shorter OS on multivariate analysis (P=0.024). However, survival differences in OS and PFS according to the disease status after the completion of chemotherapy were not observed in female patients who received upfront ASCT.
Summary
Upfront ASCT as consolidation after R-CHOP chemotherapy overcomes a negative impact of male gender and non-GCB subtype in male patients with high-risk DLBCL. Among female patients with high risk DLBCL, upfront ASCT after R-CHOP chemotherapy may overcome a negative impact of non-CR response to initial therapy. Additional data comparing with new regimens such as additional use of rituximab are necessary to find out the exact role of upfront ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL
Session topic: Publication Only
Type: Publication Only
Background
Combining rituximab to combination chemotherapy (R-CHOP) has significantly improved overall survival (OS) of patients with diffuse large B-cell lymphoma (DLBCL), but high-risk patients stratified according to the international prognostic index (IPI), non-germinal center B cells (non-GCB) subtype, and male patients have shown inferior treatment outcomes. Although the first-line treatment of patients with DLBCL is R-CHOP irrespective of the risk-group, there have been few studies evaluating the role of upfront ASCT as consolidative treatment strategy for high-risk DLBCL patients.
Aims
To investigate the role of upfront ASCT as consolidation after R-CHOP chemotherapy according to the gender in newly diagnosed advanced stage DLBCL patients.
Methods
We performed a multicenter retrospective analysis of 204 newly diagnosed DLBCL patients between January 2008 and December 2013. Patients who were younger than 65 years of age with advanced stage (Ann Arbor stage III or IV) and elevated serum lactate dehydrogenase were included. All the patients completed 4 to 8 cycles of planned R-CHOP chemotherapy and achieved at least PR after completion of planned R-CHOP chemotherapy.
Results
The median age at diagnosis was 50 (range 22-64) years and 111 (54.4%) patients were male. Median follow-up for surviving patients was 42 (range 4-115) months. Seventy-five (36.8%) patients underwent upfront ASCT as consolidation. Fifteen (11.6%) patients in the non-ASCT group (n=129) underwent ASCT after relapse. The 3-year OS and PFS rate for all patients were 78.8% and 68.4%, respectively. In multivariate analysis, non-CR after R-CHOP chemotherapy and non-upfront ASCT was associated with shorter OS (hazard ratio (HR) 2.57; 95% CI 1.34-4.95; P=0.005 and HR 2.97; 95% CI 1.38-6.40; P=0.005, respectively). Non-ASCT was also associated with shorter PFS in multivariate analysis (HR 2.26; 95% CI 1.25-4.07; P=0.014). Among the male patients, upfront ASCT showed superior OS and PFS compared to the non-ASCT group (P=0.016 and P=0.024, respectively). GCB subtype compared to the non-GCB subtype showed better PFS in male patients (P=0.026), but there were no difference in OS and PFS in male patients who received upfront ASCT. In female patients, non-CR after completion of chemotherapy was associated with shorter OS on multivariate analysis (P=0.024). However, survival differences in OS and PFS according to the disease status after the completion of chemotherapy were not observed in female patients who received upfront ASCT.
Summary
Upfront ASCT as consolidation after R-CHOP chemotherapy overcomes a negative impact of male gender and non-GCB subtype in male patients with high-risk DLBCL. Among female patients with high risk DLBCL, upfront ASCT after R-CHOP chemotherapy may overcome a negative impact of non-CR response to initial therapy. Additional data comparing with new regimens such as additional use of rituximab are necessary to find out the exact role of upfront ASCT.
Keyword(s): Autologous hematopoietic stem cell transplantation, DLBCL
Session topic: Publication Only
{{ help_message }}
{{filter}}


