
Contributions
Type: Publication Only
Background
Childhood Acute Lymphoblastic Leukemia are generally characterized by recurrent molecular and cytogenetic abnormalities; the identification of those abnormalities is clinically important because they are considered significant risk-stratifying markers.
Aims
Currently, no sufficient data exist regarding cytogenetic abnormalities and treatment outcome in Saudi pediatric ALL patients. Ninety-two cases of childhood ALL were examined to determine cytogenetic profile, and did correlations to other biologic factors.
Methods
Patients
From 2004 to 2014, we reviewed all cases with established diagnosis of childhood ALL. Of the 92 patients, 82 were B-lineage ALL, and 10 T-cell ALL. All patients were treated by UKALL 2003 protocol and risk stratified according previously published criteria.
Cytogenetic Analysis
Chromosome banding analysis and fluorescence in situ hybridization (FISH) were used to detect genetic aberrations
Analysis of FLT3 mutations
Bone marrow or blood samples were screened for FLT3 mutations (internal tandem duplications, ITDs and point mutations, D835) using polymerase chain reaction methods (PCR).
Results
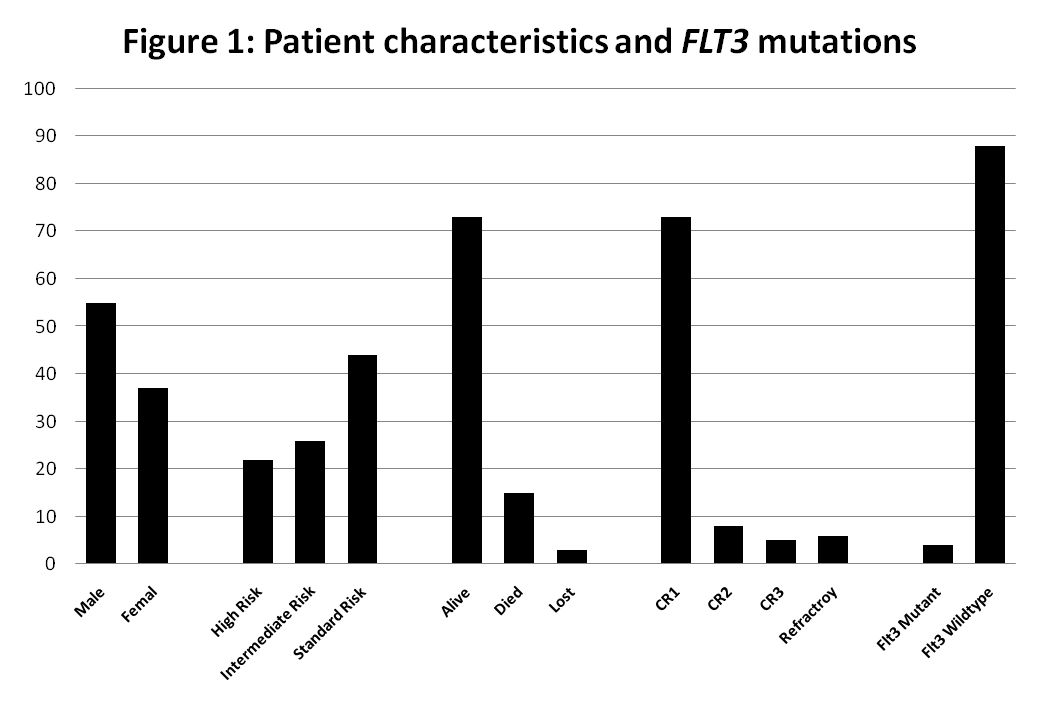
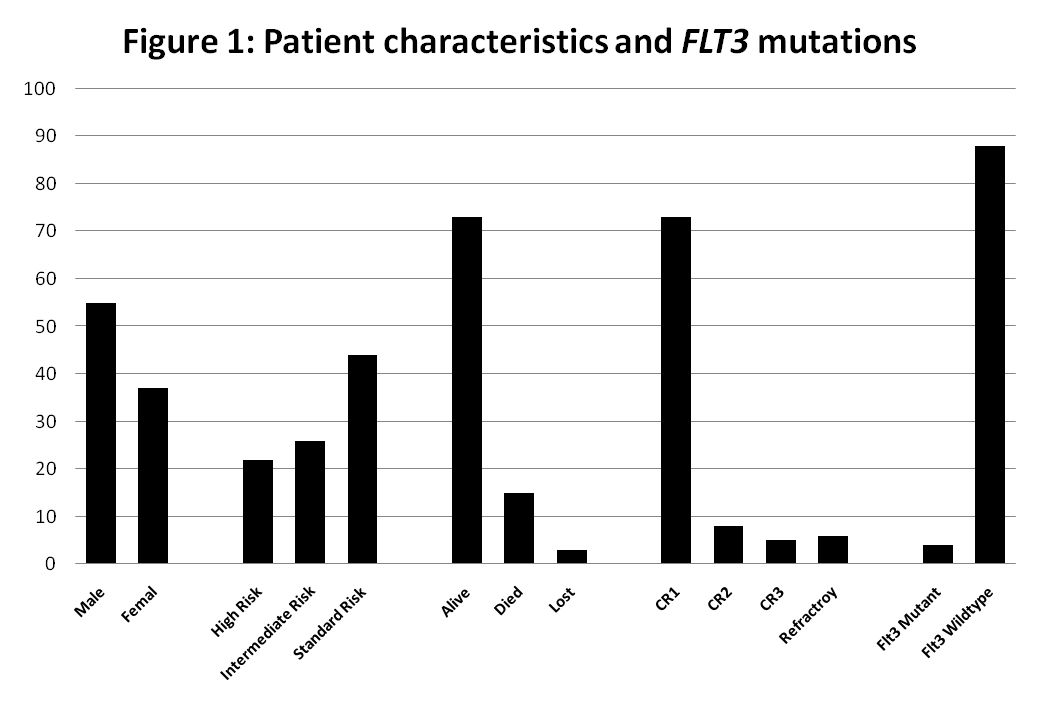
Figure 1 and table 1 Summarize patient's characteristics and patient's outcome. Cytogenetic analysis showed chromosomal anomalies in 59 out of 92 cases with overall incidence 64.1%.The most frequent chromosomal anomalies in ALL were trisomy 21, t(9;22), and t(12;21). Our data are in accordance with those published showed that FLT3 mutations not common in ALL patients (4.7%) and have no prognostic relevance in pediatric ALL patients while t(9;22) and MLL gene rearrangements were signs of a bad prognosis in childhood ALL, with high rate of relapse, shorter overall survival; (P=0.031) and event-free survival (EFS) was also worse(P=0.040) compared to standard risk group.
Table 1: Cytogentic abnormalities detected in our study
Available for Karyotype | 28 normal |
Available for Fish | n=83 |
t (9;22) | 10 (12%) |
t (12;21) | 8 (9.6%) |
MLL | 6 (7.2%) |
MYC | 2 (2.4%) |
t (1;19) | 1 (1.2%) |
+21 | 11 (13.3%) |
Del 12p | 5 (6%) |
+6 | 1 (1.2%) |
+9 | 3 (4.6%) |
+8 | 1 (1.2%) |
-19 | 1 (1.2%) |
Hyperdiploid | 6 (7.3%) |
Pseudotriploidy | 2 (3.1%) |
tetraploidy | 1 (1.5%) |
Summary
Our data are in accordance with those published and confirm that the frequency of cytogenetic abnormalities and their prognostic relevant were comparable to those reported in the literature. FLT3 mutations not common among Saudi ALL and occur in low percentage and had no prognostic relevance as in AML and did not affect clinical outcome.
Keyword(s): Acute lymphoblastic leukemia, Cytogenetic abnormalities, FLT3, Outcome
Session topic: Publication Only
Type: Publication Only
Background
Childhood Acute Lymphoblastic Leukemia are generally characterized by recurrent molecular and cytogenetic abnormalities; the identification of those abnormalities is clinically important because they are considered significant risk-stratifying markers.
Aims
Currently, no sufficient data exist regarding cytogenetic abnormalities and treatment outcome in Saudi pediatric ALL patients. Ninety-two cases of childhood ALL were examined to determine cytogenetic profile, and did correlations to other biologic factors.
Methods
Patients
From 2004 to 2014, we reviewed all cases with established diagnosis of childhood ALL. Of the 92 patients, 82 were B-lineage ALL, and 10 T-cell ALL. All patients were treated by UKALL 2003 protocol and risk stratified according previously published criteria.
Cytogenetic Analysis
Chromosome banding analysis and fluorescence in situ hybridization (FISH) were used to detect genetic aberrations
Analysis of FLT3 mutations
Bone marrow or blood samples were screened for FLT3 mutations (internal tandem duplications, ITDs and point mutations, D835) using polymerase chain reaction methods (PCR).
Results
Figure 1 and table 1 Summarize patient's characteristics and patient's outcome. Cytogenetic analysis showed chromosomal anomalies in 59 out of 92 cases with overall incidence 64.1%.The most frequent chromosomal anomalies in ALL were trisomy 21, t(9;22), and t(12;21). Our data are in accordance with those published showed that FLT3 mutations not common in ALL patients (4.7%) and have no prognostic relevance in pediatric ALL patients while t(9;22) and MLL gene rearrangements were signs of a bad prognosis in childhood ALL, with high rate of relapse, shorter overall survival; (P=0.031) and event-free survival (EFS) was also worse(P=0.040) compared to standard risk group.
Table 1: Cytogentic abnormalities detected in our study
Available for Karyotype | 28 normal |
Available for Fish | n=83 |
t (9;22) | 10 (12%) |
t (12;21) | 8 (9.6%) |
MLL | 6 (7.2%) |
MYC | 2 (2.4%) |
t (1;19) | 1 (1.2%) |
+21 | 11 (13.3%) |
Del 12p | 5 (6%) |
+6 | 1 (1.2%) |
+9 | 3 (4.6%) |
+8 | 1 (1.2%) |
-19 | 1 (1.2%) |
Hyperdiploid | 6 (7.3%) |
Pseudotriploidy | 2 (3.1%) |
tetraploidy | 1 (1.5%) |
Summary
Our data are in accordance with those published and confirm that the frequency of cytogenetic abnormalities and their prognostic relevant were comparable to those reported in the literature. FLT3 mutations not common among Saudi ALL and occur in low percentage and had no prognostic relevance as in AML and did not affect clinical outcome.
Keyword(s): Acute lymphoblastic leukemia, Cytogenetic abnormalities, FLT3, Outcome
Session topic: Publication Only


