TREATING HIV-RELATED NON-HODGKIN LYMPHOMA IN SEVERELY IMMUNOCOMPROMISED PATIENTS, IN THE CART ERA. A SINGLE CENTER EXPERIENCE.
(Abstract release date: 05/21/15)
EHA Library. Re A. 06/12/15; 102954; PB1671
Disclosure(s): SPEDALI CIVILI DI BRESCIA
Alessandro Re
Contributions
Contributions
Abstract
Abstract: PB1671
Type: Publication Only
Background
Low CD4+ lymphocyte count at diagnosis, in patients (pts) with HIV-related non-Hodgkin’s lymphoma (NHL), is associated with poor clinical outcome, mainly due to low treatment tolerability. Severely immunocompromised pts are frequently excluded from clinical trials. Moreover, several authors claim that Rituximab should be held in pts with very low CD4 count due to the increased risk of infections
Aims
To define the outcome of severely immunocompromised HIV positive (+) pts with NHL in the real-life, in terms of possibility to receive treatment with curative intent, treatment-related mortality (TRM), complete remission (CR) rate and survival
Methods
All consecutive HIV pos pts diagnosed at our Institution from Jan 1997 to Dec 2013 (cART era) with aggressive systemic NHL and CD4+ lymphocyte count <100/mcl (CD4<100) at lymphoma diagnosis were considered. Histology included DLBCL, Burkitt, plasmablastic or other aggressive lymphomas. Pts’characteristics, treatment response and long-term outcome were compared with the concomitant series of HIV-related NHL pts with CD4+ lymphocyte count >100/mcl (CD4>100). Each pt was treated with standard state-of-the art in lymphoma and HIV care at the time of diagnosis, or enrolled in prospective trials. After 2001 all pts with CD20+ NHL received Rituximab combining chemotherapy (CT)
Results
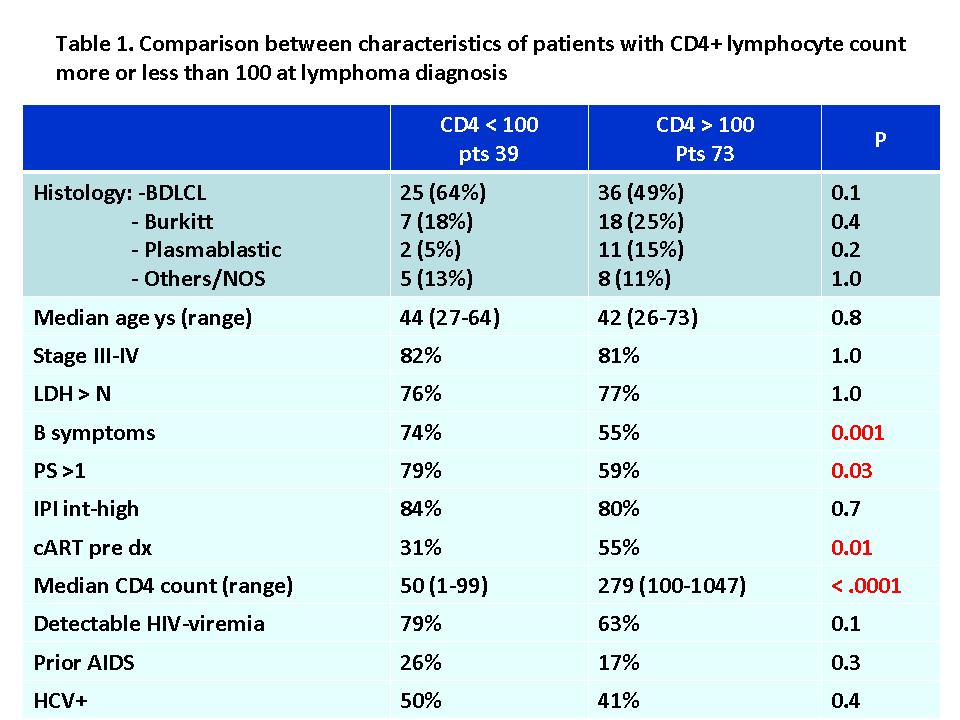
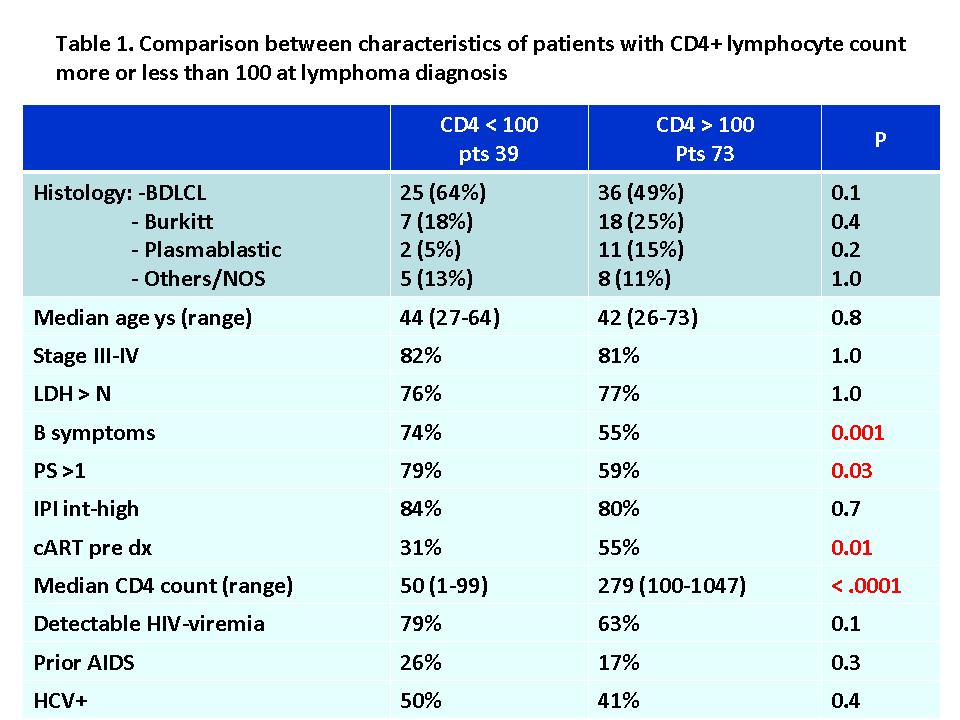
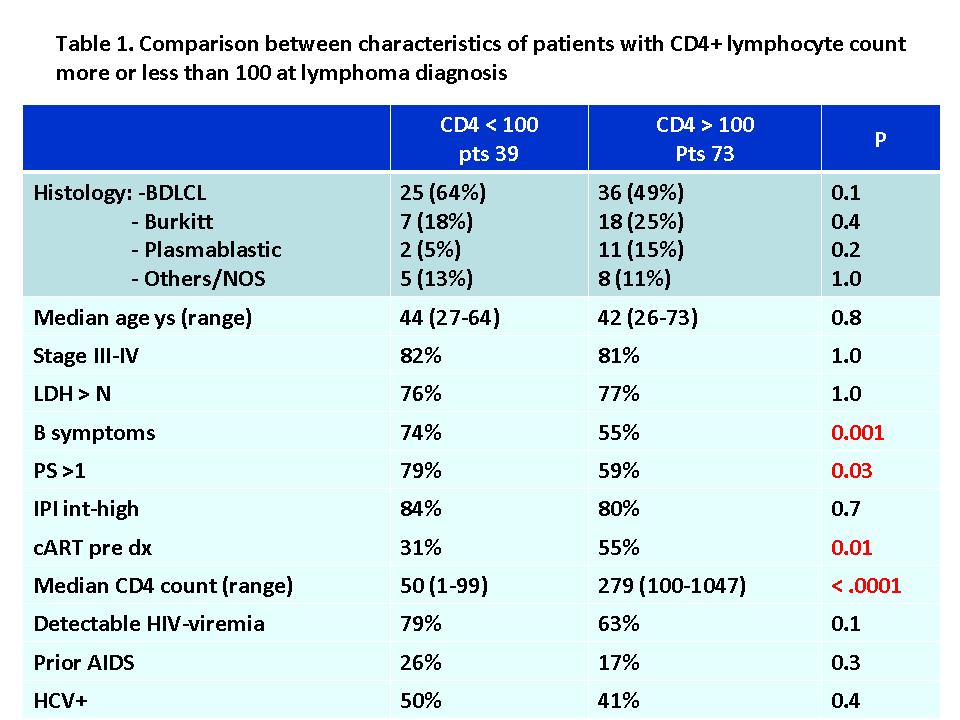
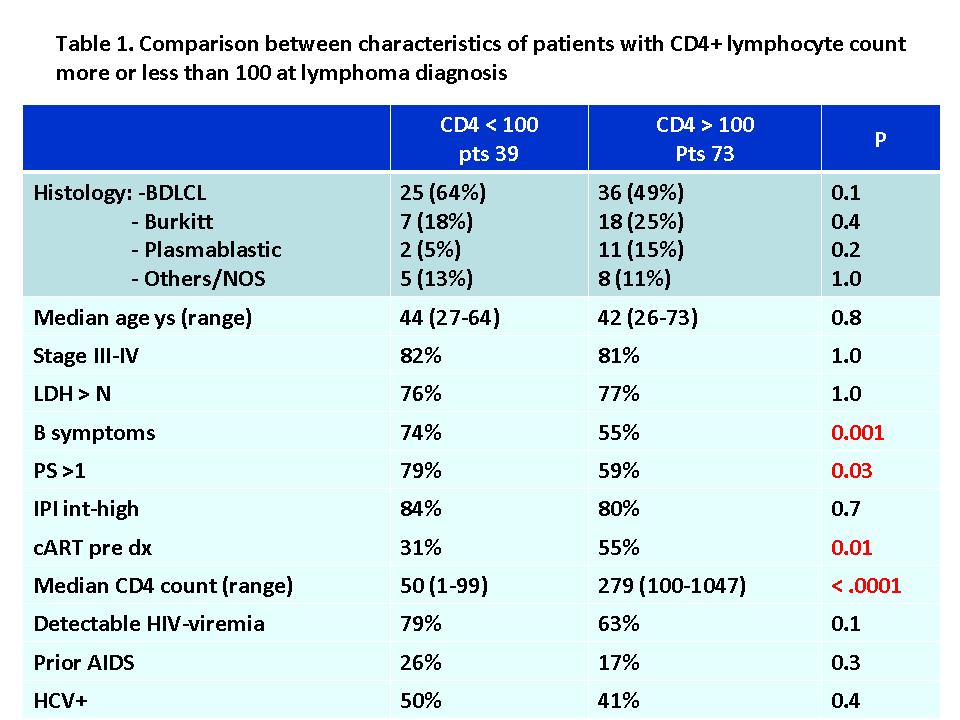
Since 1985 to 2013 198 HIV pos pts were diagnosed at our Institution with NHL, 84 in the pre-cART era (1985-1996) and 114 in the cART era (1997-2013). The proportion of pts with CD4<100 during the cART era was 35% vs 63% in the pre-cART era (P=.0002). The clinical characteristics of the 2 groups (CD4>100 vs CD4<100) are shown in table 1. Significant differences included worse performance status (PS) and more pts with B symptoms in CD4<100 group and a greater proportion of pts on cART at NHL onset in CD4>100 group. The proportion of pts with CD4<100 we treated with curative intent was 63% vs 97% in pts with CD4>100 (P<0.0001). Pts were excluded from curative treatment for poor PS, major infections and/or severe comorbidities. After a follow-up of 60 ms (1-204), the 5y-overall survival (OS) of the 2 groups of pts was 31% (CD4<100) and 60% (CD4>100) (P=0.003). However, analysing pts who underwent CT, CR rate was similar (54% for CD4 <100 and 64% in CD4>100; P= 0.6). TRM was respectively 21% and 9% and included mainly infectious events. Overall, 14 pts (58%) died in CD4<100 (cause of death: NHL 7 pts,TRM 5,HCV cirrosis 1 and unknown 1) and 29 (41%) in CD4>100 group (NHL 19,TRM 6,lung cancer 1,car crush 1,suicide 1 and drug overdose 1). Response duration was not different (85% and 84% at 5 years). A trend towards worse OS and PFS were seen in pts treated with CD4<100 (38% vs 62% and 39% vs 52%) (P=NS). Fifteen pts with CD4<100 (DLBCL 11 and Burkitt 4) received Rituximab combining CT, while 6 pts (DLBCL 5 and Burkitt 1) did not. The CR rate for pts who received Rituximab was higher (60% vs 33%, P=NS) with similar TRM (20% vs 17%), and median OS and PFS of 19 vs 4.5 ms and 17 vs 4.5 ms (P=NS)
Summary
After the advent of cART the proportion of severely immunocompromised pts with HIV-related NHL has significantly decreased. In our single center experience, a substantial proportion of them could not receive adequate treatment and OS remained poor. However, if properly treated with standard immunochemotherapy, the CR rate was similar to pts with less immunocompromise, with chance of favourable long-term outcome. TRM was not negligible. Rituximab appears feasible in this setting and it seems to improve CR rate and possibility of long-term survival
Keyword(s): HIV, Non-Hodgkin's lymphoma
Session topic: Publication Only
Type: Publication Only
Background
Low CD4+ lymphocyte count at diagnosis, in patients (pts) with HIV-related non-Hodgkin’s lymphoma (NHL), is associated with poor clinical outcome, mainly due to low treatment tolerability. Severely immunocompromised pts are frequently excluded from clinical trials. Moreover, several authors claim that Rituximab should be held in pts with very low CD4 count due to the increased risk of infections
Aims
To define the outcome of severely immunocompromised HIV positive (+) pts with NHL in the real-life, in terms of possibility to receive treatment with curative intent, treatment-related mortality (TRM), complete remission (CR) rate and survival
Methods
All consecutive HIV pos pts diagnosed at our Institution from Jan 1997 to Dec 2013 (cART era) with aggressive systemic NHL and CD4+ lymphocyte count <100/mcl (CD4<100) at lymphoma diagnosis were considered. Histology included DLBCL, Burkitt, plasmablastic or other aggressive lymphomas. Pts’characteristics, treatment response and long-term outcome were compared with the concomitant series of HIV-related NHL pts with CD4+ lymphocyte count >100/mcl (CD4>100). Each pt was treated with standard state-of-the art in lymphoma and HIV care at the time of diagnosis, or enrolled in prospective trials. After 2001 all pts with CD20+ NHL received Rituximab combining chemotherapy (CT)
Results
Since 1985 to 2013 198 HIV pos pts were diagnosed at our Institution with NHL, 84 in the pre-cART era (1985-1996) and 114 in the cART era (1997-2013). The proportion of pts with CD4<100 during the cART era was 35% vs 63% in the pre-cART era (P=.0002). The clinical characteristics of the 2 groups (CD4>100 vs CD4<100) are shown in table 1. Significant differences included worse performance status (PS) and more pts with B symptoms in CD4<100 group and a greater proportion of pts on cART at NHL onset in CD4>100 group. The proportion of pts with CD4<100 we treated with curative intent was 63% vs 97% in pts with CD4>100 (P<0.0001). Pts were excluded from curative treatment for poor PS, major infections and/or severe comorbidities. After a follow-up of 60 ms (1-204), the 5y-overall survival (OS) of the 2 groups of pts was 31% (CD4<100) and 60% (CD4>100) (P=0.003). However, analysing pts who underwent CT, CR rate was similar (54% for CD4 <100 and 64% in CD4>100; P= 0.6). TRM was respectively 21% and 9% and included mainly infectious events. Overall, 14 pts (58%) died in CD4<100 (cause of death: NHL 7 pts,TRM 5,HCV cirrosis 1 and unknown 1) and 29 (41%) in CD4>100 group (NHL 19,TRM 6,lung cancer 1,car crush 1,suicide 1 and drug overdose 1). Response duration was not different (85% and 84% at 5 years). A trend towards worse OS and PFS were seen in pts treated with CD4<100 (38% vs 62% and 39% vs 52%) (P=NS). Fifteen pts with CD4<100 (DLBCL 11 and Burkitt 4) received Rituximab combining CT, while 6 pts (DLBCL 5 and Burkitt 1) did not. The CR rate for pts who received Rituximab was higher (60% vs 33%, P=NS) with similar TRM (20% vs 17%), and median OS and PFS of 19 vs 4.5 ms and 17 vs 4.5 ms (P=NS)
Summary
After the advent of cART the proportion of severely immunocompromised pts with HIV-related NHL has significantly decreased. In our single center experience, a substantial proportion of them could not receive adequate treatment and OS remained poor. However, if properly treated with standard immunochemotherapy, the CR rate was similar to pts with less immunocompromise, with chance of favourable long-term outcome. TRM was not negligible. Rituximab appears feasible in this setting and it seems to improve CR rate and possibility of long-term survival
Keyword(s): HIV, Non-Hodgkin's lymphoma
Session topic: Publication Only
Abstract: PB1671
Type: Publication Only
Background
Low CD4+ lymphocyte count at diagnosis, in patients (pts) with HIV-related non-Hodgkin’s lymphoma (NHL), is associated with poor clinical outcome, mainly due to low treatment tolerability. Severely immunocompromised pts are frequently excluded from clinical trials. Moreover, several authors claim that Rituximab should be held in pts with very low CD4 count due to the increased risk of infections
Aims
To define the outcome of severely immunocompromised HIV positive (+) pts with NHL in the real-life, in terms of possibility to receive treatment with curative intent, treatment-related mortality (TRM), complete remission (CR) rate and survival
Methods
All consecutive HIV pos pts diagnosed at our Institution from Jan 1997 to Dec 2013 (cART era) with aggressive systemic NHL and CD4+ lymphocyte count <100/mcl (CD4<100) at lymphoma diagnosis were considered. Histology included DLBCL, Burkitt, plasmablastic or other aggressive lymphomas. Pts’characteristics, treatment response and long-term outcome were compared with the concomitant series of HIV-related NHL pts with CD4+ lymphocyte count >100/mcl (CD4>100). Each pt was treated with standard state-of-the art in lymphoma and HIV care at the time of diagnosis, or enrolled in prospective trials. After 2001 all pts with CD20+ NHL received Rituximab combining chemotherapy (CT)
Results
Since 1985 to 2013 198 HIV pos pts were diagnosed at our Institution with NHL, 84 in the pre-cART era (1985-1996) and 114 in the cART era (1997-2013). The proportion of pts with CD4<100 during the cART era was 35% vs 63% in the pre-cART era (P=.0002). The clinical characteristics of the 2 groups (CD4>100 vs CD4<100) are shown in table 1. Significant differences included worse performance status (PS) and more pts with B symptoms in CD4<100 group and a greater proportion of pts on cART at NHL onset in CD4>100 group. The proportion of pts with CD4<100 we treated with curative intent was 63% vs 97% in pts with CD4>100 (P<0.0001). Pts were excluded from curative treatment for poor PS, major infections and/or severe comorbidities. After a follow-up of 60 ms (1-204), the 5y-overall survival (OS) of the 2 groups of pts was 31% (CD4<100) and 60% (CD4>100) (P=0.003). However, analysing pts who underwent CT, CR rate was similar (54% for CD4 <100 and 64% in CD4>100; P= 0.6). TRM was respectively 21% and 9% and included mainly infectious events. Overall, 14 pts (58%) died in CD4<100 (cause of death: NHL 7 pts,TRM 5,HCV cirrosis 1 and unknown 1) and 29 (41%) in CD4>100 group (NHL 19,TRM 6,lung cancer 1,car crush 1,suicide 1 and drug overdose 1). Response duration was not different (85% and 84% at 5 years). A trend towards worse OS and PFS were seen in pts treated with CD4<100 (38% vs 62% and 39% vs 52%) (P=NS). Fifteen pts with CD4<100 (DLBCL 11 and Burkitt 4) received Rituximab combining CT, while 6 pts (DLBCL 5 and Burkitt 1) did not. The CR rate for pts who received Rituximab was higher (60% vs 33%, P=NS) with similar TRM (20% vs 17%), and median OS and PFS of 19 vs 4.5 ms and 17 vs 4.5 ms (P=NS)
Summary
After the advent of cART the proportion of severely immunocompromised pts with HIV-related NHL has significantly decreased. In our single center experience, a substantial proportion of them could not receive adequate treatment and OS remained poor. However, if properly treated with standard immunochemotherapy, the CR rate was similar to pts with less immunocompromise, with chance of favourable long-term outcome. TRM was not negligible. Rituximab appears feasible in this setting and it seems to improve CR rate and possibility of long-term survival
Keyword(s): HIV, Non-Hodgkin's lymphoma
Session topic: Publication Only
Type: Publication Only
Background
Low CD4+ lymphocyte count at diagnosis, in patients (pts) with HIV-related non-Hodgkin’s lymphoma (NHL), is associated with poor clinical outcome, mainly due to low treatment tolerability. Severely immunocompromised pts are frequently excluded from clinical trials. Moreover, several authors claim that Rituximab should be held in pts with very low CD4 count due to the increased risk of infections
Aims
To define the outcome of severely immunocompromised HIV positive (+) pts with NHL in the real-life, in terms of possibility to receive treatment with curative intent, treatment-related mortality (TRM), complete remission (CR) rate and survival
Methods
All consecutive HIV pos pts diagnosed at our Institution from Jan 1997 to Dec 2013 (cART era) with aggressive systemic NHL and CD4+ lymphocyte count <100/mcl (CD4<100) at lymphoma diagnosis were considered. Histology included DLBCL, Burkitt, plasmablastic or other aggressive lymphomas. Pts’characteristics, treatment response and long-term outcome were compared with the concomitant series of HIV-related NHL pts with CD4+ lymphocyte count >100/mcl (CD4>100). Each pt was treated with standard state-of-the art in lymphoma and HIV care at the time of diagnosis, or enrolled in prospective trials. After 2001 all pts with CD20+ NHL received Rituximab combining chemotherapy (CT)
Results
Since 1985 to 2013 198 HIV pos pts were diagnosed at our Institution with NHL, 84 in the pre-cART era (1985-1996) and 114 in the cART era (1997-2013). The proportion of pts with CD4<100 during the cART era was 35% vs 63% in the pre-cART era (P=.0002). The clinical characteristics of the 2 groups (CD4>100 vs CD4<100) are shown in table 1. Significant differences included worse performance status (PS) and more pts with B symptoms in CD4<100 group and a greater proportion of pts on cART at NHL onset in CD4>100 group. The proportion of pts with CD4<100 we treated with curative intent was 63% vs 97% in pts with CD4>100 (P<0.0001). Pts were excluded from curative treatment for poor PS, major infections and/or severe comorbidities. After a follow-up of 60 ms (1-204), the 5y-overall survival (OS) of the 2 groups of pts was 31% (CD4<100) and 60% (CD4>100) (P=0.003). However, analysing pts who underwent CT, CR rate was similar (54% for CD4 <100 and 64% in CD4>100; P= 0.6). TRM was respectively 21% and 9% and included mainly infectious events. Overall, 14 pts (58%) died in CD4<100 (cause of death: NHL 7 pts,TRM 5,HCV cirrosis 1 and unknown 1) and 29 (41%) in CD4>100 group (NHL 19,TRM 6,lung cancer 1,car crush 1,suicide 1 and drug overdose 1). Response duration was not different (85% and 84% at 5 years). A trend towards worse OS and PFS were seen in pts treated with CD4<100 (38% vs 62% and 39% vs 52%) (P=NS). Fifteen pts with CD4<100 (DLBCL 11 and Burkitt 4) received Rituximab combining CT, while 6 pts (DLBCL 5 and Burkitt 1) did not. The CR rate for pts who received Rituximab was higher (60% vs 33%, P=NS) with similar TRM (20% vs 17%), and median OS and PFS of 19 vs 4.5 ms and 17 vs 4.5 ms (P=NS)
Summary
After the advent of cART the proportion of severely immunocompromised pts with HIV-related NHL has significantly decreased. In our single center experience, a substantial proportion of them could not receive adequate treatment and OS remained poor. However, if properly treated with standard immunochemotherapy, the CR rate was similar to pts with less immunocompromise, with chance of favourable long-term outcome. TRM was not negligible. Rituximab appears feasible in this setting and it seems to improve CR rate and possibility of long-term survival
Keyword(s): HIV, Non-Hodgkin's lymphoma
Session topic: Publication Only
{{ help_message }}
{{filter}}


