COMBINATION OF CHEMOTHERAPY AND RADIATION IMPROVE THE PROGNOSIS OF PRIMARY DIFFUSE LARGE B-CELL LYMPHOMA OF THE TONSIL.
(Abstract release date: 05/21/15)
EHA Library. Lim S. 06/12/15; 102930; PB1670
Disclosure(s): Haeundae Paik HospitalInternal Medicine

Dr. Sungnam Lim
Contributions
Contributions
Abstract
Abstract: PB1670
Type: Publication Only
Background
Non-Hodgkin lymphoma of the Waldeyer’s ring is a relatively rare entity and the tonsil is the most frequently involved site. The majority of tonsil lymphomas are of B-cell origin and the most common histological type is diffuse large B-cell lymphoma (DLBCL). Treatment approaches that have used include chemotherapy (CTx) alone, radiation (RT) alone, and combination of both.
Aims
We reviewed our data and evaluate treatment outcome of patient with primary diffuse large B-cell lymphoma of the tonsil.
Methods
Retrospective review of 114 stage I-II DLBCL patients treated with curative intent between 1995 and 2010. Forty-five (39.5%) patients had stage I disease and systemic symptoms (B-symptoms) were present in only 7 (6%) patients. Seventy-two (65.5%) patients were treated with CTx alone, whereas the remaining 38 (34.5%) received treatment with a combination of CTx and RT. Chemotherapy was CHOP-based, with R-CHOP in 80 patients (70%). Median involved-field RT dose was 3,960 cGy, with 96% receiving more than 3,000 cGy.
Results
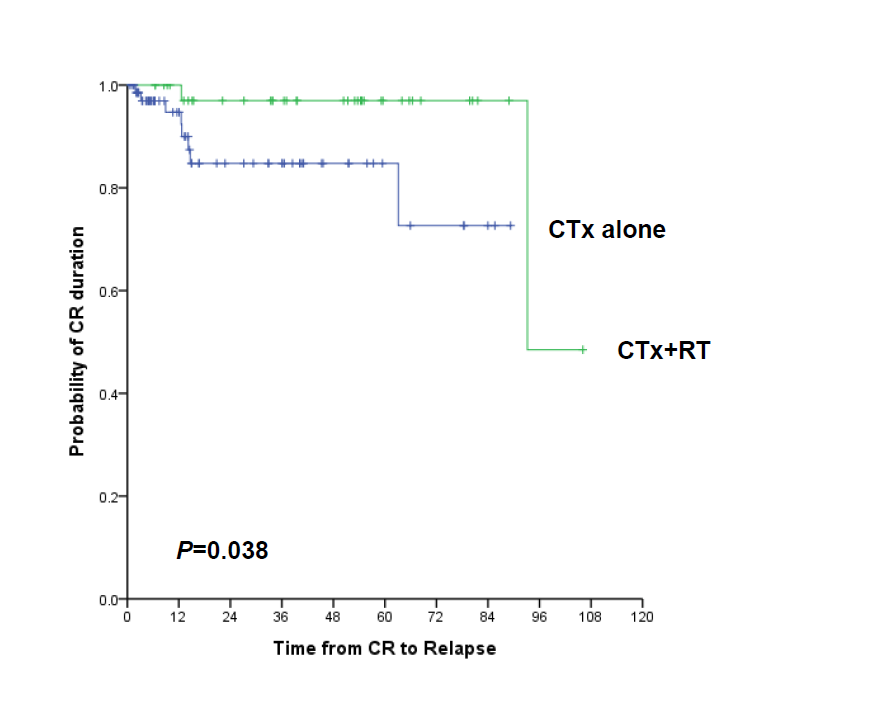
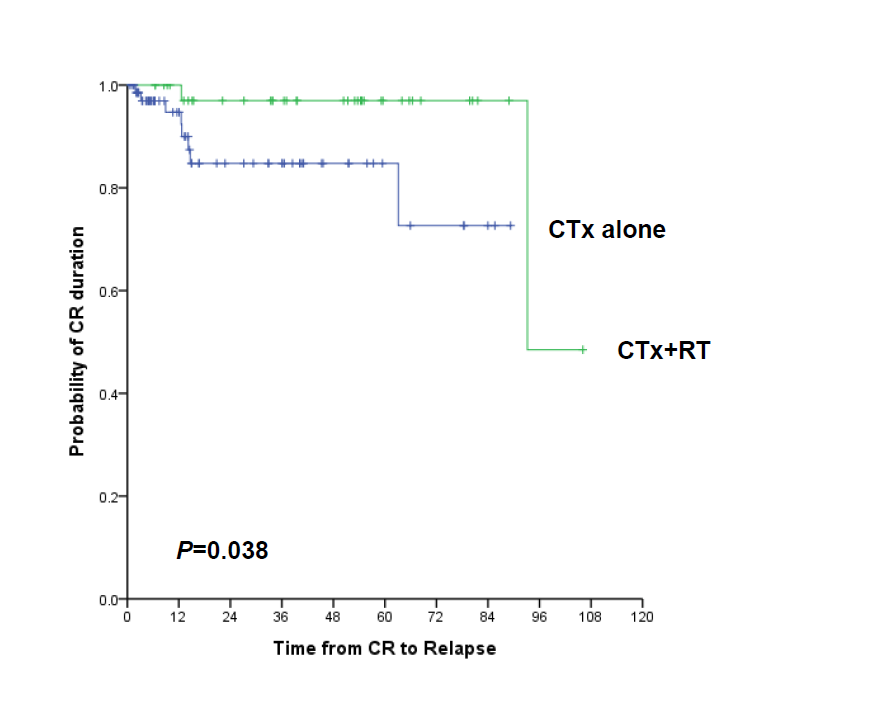
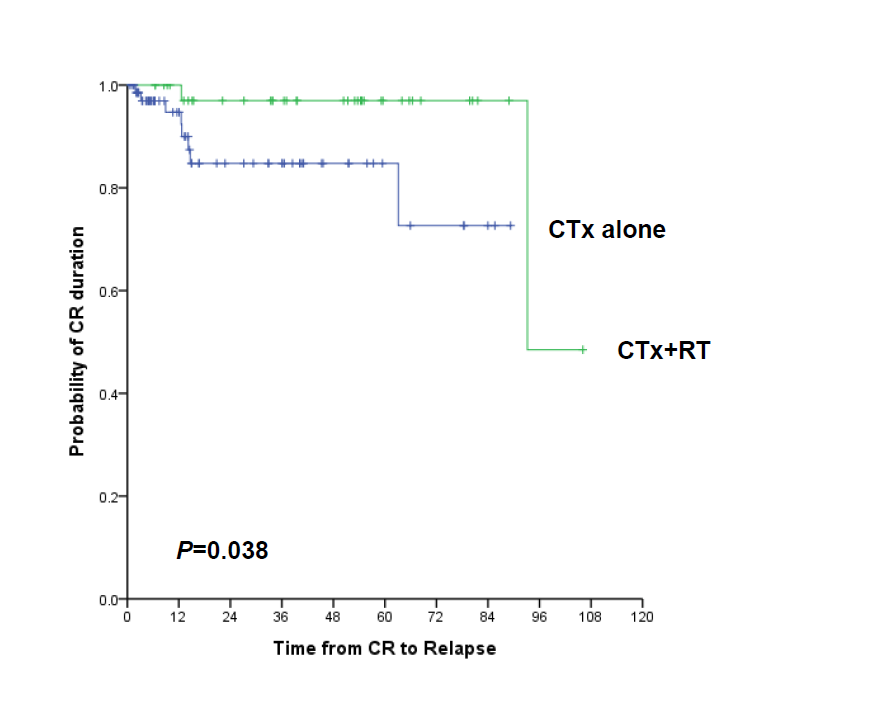
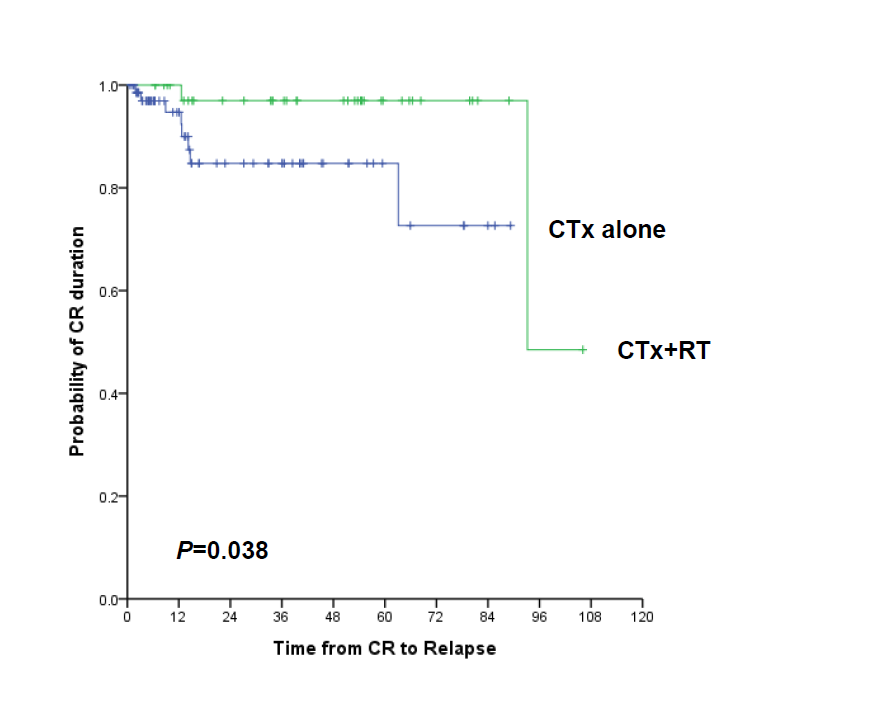
The median age was 59 years and the majority of patients (61%) were males. Low risk disease: low to low intermediate by International prognostic index (IPI) was 97.3% and only 10 (8.8%) patients had high serum lactate dehydrogenase (LDH) level. Overall CR rate was 73.5% and seven (13.5%) of the patients who had achieved CR had recurred. The median follow up was 28 months (34 months for CHOP-treated, 23 months for R-CHOP). Disease-free survival (DFS) and overall survival (OS) were 43.9% and 42.5%, respectively. Significant prognostic factors included: age ≥60 year-old (OS: 93.1% vs. 74.1%, P=0.011; DFS: 83.3% vs. 80.6%, P=0.160), LDH >upper normal limit (OS: 88.2% vs. 72.9%, P=0.003; DFS: 86.8% vs.20.0%, P<0.001), IPI>0 (OS: 90.0% vs. 55.9%, P=0.007; DFS: 86.5% vs. 64.0%, P=0.034) and combination of CTx and RT (OS: 79.6% vs. 48.2%, P=0.025; DFS: 72.6% vs. 48.5%, P=0.038). Germinal center (GC) and non-GC phenotype were not predictors of outcome in localized primary DLBCL of the tonsil. Combination chemotherapy-treated patients with rituximab did not show a significantly better OS and DFS than the combination chemotherapy-treated patients without rituximab. On multivariate analysis; LDH >upper normal limit (DFS: hazard ratio [HR], 14.958; 95% CI, 2.474-90.432, P=0.003; OS: HR, 9.341; 95% CI, 1.635-53.361, P=0.012), and combination of CTx and RT (DFS: HR, 0.088: 95% CI, 0.009-0.834, P=0.034; OS: HR, 0.112; 95% CI, 0.014-0.918, P=0.041), retained statistical significance.
Summary
The DFS and OS rates were significantly better for patients receiving combination of CTx and RT. A combined treatment, consisting of CTx and RT results in a satisfactory outcome in patients with localized primary DLBCL of tonsil.
Keyword(s): Chemotherapy, Diffuse large B cell lymphoma, Radiotherapy
Session topic: Publication Only
Type: Publication Only
Background
Non-Hodgkin lymphoma of the Waldeyer’s ring is a relatively rare entity and the tonsil is the most frequently involved site. The majority of tonsil lymphomas are of B-cell origin and the most common histological type is diffuse large B-cell lymphoma (DLBCL). Treatment approaches that have used include chemotherapy (CTx) alone, radiation (RT) alone, and combination of both.
Aims
We reviewed our data and evaluate treatment outcome of patient with primary diffuse large B-cell lymphoma of the tonsil.
Methods
Retrospective review of 114 stage I-II DLBCL patients treated with curative intent between 1995 and 2010. Forty-five (39.5%) patients had stage I disease and systemic symptoms (B-symptoms) were present in only 7 (6%) patients. Seventy-two (65.5%) patients were treated with CTx alone, whereas the remaining 38 (34.5%) received treatment with a combination of CTx and RT. Chemotherapy was CHOP-based, with R-CHOP in 80 patients (70%). Median involved-field RT dose was 3,960 cGy, with 96% receiving more than 3,000 cGy.
Results
The median age was 59 years and the majority of patients (61%) were males. Low risk disease: low to low intermediate by International prognostic index (IPI) was 97.3% and only 10 (8.8%) patients had high serum lactate dehydrogenase (LDH) level. Overall CR rate was 73.5% and seven (13.5%) of the patients who had achieved CR had recurred. The median follow up was 28 months (34 months for CHOP-treated, 23 months for R-CHOP). Disease-free survival (DFS) and overall survival (OS) were 43.9% and 42.5%, respectively. Significant prognostic factors included: age ≥60 year-old (OS: 93.1% vs. 74.1%, P=0.011; DFS: 83.3% vs. 80.6%, P=0.160), LDH >upper normal limit (OS: 88.2% vs. 72.9%, P=0.003; DFS: 86.8% vs.20.0%, P<0.001), IPI>0 (OS: 90.0% vs. 55.9%, P=0.007; DFS: 86.5% vs. 64.0%, P=0.034) and combination of CTx and RT (OS: 79.6% vs. 48.2%, P=0.025; DFS: 72.6% vs. 48.5%, P=0.038). Germinal center (GC) and non-GC phenotype were not predictors of outcome in localized primary DLBCL of the tonsil. Combination chemotherapy-treated patients with rituximab did not show a significantly better OS and DFS than the combination chemotherapy-treated patients without rituximab. On multivariate analysis; LDH >upper normal limit (DFS: hazard ratio [HR], 14.958; 95% CI, 2.474-90.432, P=0.003; OS: HR, 9.341; 95% CI, 1.635-53.361, P=0.012), and combination of CTx and RT (DFS: HR, 0.088: 95% CI, 0.009-0.834, P=0.034; OS: HR, 0.112; 95% CI, 0.014-0.918, P=0.041), retained statistical significance.
Summary
The DFS and OS rates were significantly better for patients receiving combination of CTx and RT. A combined treatment, consisting of CTx and RT results in a satisfactory outcome in patients with localized primary DLBCL of tonsil.
Keyword(s): Chemotherapy, Diffuse large B cell lymphoma, Radiotherapy
Session topic: Publication Only
Abstract: PB1670
Type: Publication Only
Background
Non-Hodgkin lymphoma of the Waldeyer’s ring is a relatively rare entity and the tonsil is the most frequently involved site. The majority of tonsil lymphomas are of B-cell origin and the most common histological type is diffuse large B-cell lymphoma (DLBCL). Treatment approaches that have used include chemotherapy (CTx) alone, radiation (RT) alone, and combination of both.
Aims
We reviewed our data and evaluate treatment outcome of patient with primary diffuse large B-cell lymphoma of the tonsil.
Methods
Retrospective review of 114 stage I-II DLBCL patients treated with curative intent between 1995 and 2010. Forty-five (39.5%) patients had stage I disease and systemic symptoms (B-symptoms) were present in only 7 (6%) patients. Seventy-two (65.5%) patients were treated with CTx alone, whereas the remaining 38 (34.5%) received treatment with a combination of CTx and RT. Chemotherapy was CHOP-based, with R-CHOP in 80 patients (70%). Median involved-field RT dose was 3,960 cGy, with 96% receiving more than 3,000 cGy.
Results
The median age was 59 years and the majority of patients (61%) were males. Low risk disease: low to low intermediate by International prognostic index (IPI) was 97.3% and only 10 (8.8%) patients had high serum lactate dehydrogenase (LDH) level. Overall CR rate was 73.5% and seven (13.5%) of the patients who had achieved CR had recurred. The median follow up was 28 months (34 months for CHOP-treated, 23 months for R-CHOP). Disease-free survival (DFS) and overall survival (OS) were 43.9% and 42.5%, respectively. Significant prognostic factors included: age ≥60 year-old (OS: 93.1% vs. 74.1%, P=0.011; DFS: 83.3% vs. 80.6%, P=0.160), LDH >upper normal limit (OS: 88.2% vs. 72.9%, P=0.003; DFS: 86.8% vs.20.0%, P<0.001), IPI>0 (OS: 90.0% vs. 55.9%, P=0.007; DFS: 86.5% vs. 64.0%, P=0.034) and combination of CTx and RT (OS: 79.6% vs. 48.2%, P=0.025; DFS: 72.6% vs. 48.5%, P=0.038). Germinal center (GC) and non-GC phenotype were not predictors of outcome in localized primary DLBCL of the tonsil. Combination chemotherapy-treated patients with rituximab did not show a significantly better OS and DFS than the combination chemotherapy-treated patients without rituximab. On multivariate analysis; LDH >upper normal limit (DFS: hazard ratio [HR], 14.958; 95% CI, 2.474-90.432, P=0.003; OS: HR, 9.341; 95% CI, 1.635-53.361, P=0.012), and combination of CTx and RT (DFS: HR, 0.088: 95% CI, 0.009-0.834, P=0.034; OS: HR, 0.112; 95% CI, 0.014-0.918, P=0.041), retained statistical significance.
Summary
The DFS and OS rates were significantly better for patients receiving combination of CTx and RT. A combined treatment, consisting of CTx and RT results in a satisfactory outcome in patients with localized primary DLBCL of tonsil.
Keyword(s): Chemotherapy, Diffuse large B cell lymphoma, Radiotherapy
Session topic: Publication Only
Type: Publication Only
Background
Non-Hodgkin lymphoma of the Waldeyer’s ring is a relatively rare entity and the tonsil is the most frequently involved site. The majority of tonsil lymphomas are of B-cell origin and the most common histological type is diffuse large B-cell lymphoma (DLBCL). Treatment approaches that have used include chemotherapy (CTx) alone, radiation (RT) alone, and combination of both.
Aims
We reviewed our data and evaluate treatment outcome of patient with primary diffuse large B-cell lymphoma of the tonsil.
Methods
Retrospective review of 114 stage I-II DLBCL patients treated with curative intent between 1995 and 2010. Forty-five (39.5%) patients had stage I disease and systemic symptoms (B-symptoms) were present in only 7 (6%) patients. Seventy-two (65.5%) patients were treated with CTx alone, whereas the remaining 38 (34.5%) received treatment with a combination of CTx and RT. Chemotherapy was CHOP-based, with R-CHOP in 80 patients (70%). Median involved-field RT dose was 3,960 cGy, with 96% receiving more than 3,000 cGy.
Results
The median age was 59 years and the majority of patients (61%) were males. Low risk disease: low to low intermediate by International prognostic index (IPI) was 97.3% and only 10 (8.8%) patients had high serum lactate dehydrogenase (LDH) level. Overall CR rate was 73.5% and seven (13.5%) of the patients who had achieved CR had recurred. The median follow up was 28 months (34 months for CHOP-treated, 23 months for R-CHOP). Disease-free survival (DFS) and overall survival (OS) were 43.9% and 42.5%, respectively. Significant prognostic factors included: age ≥60 year-old (OS: 93.1% vs. 74.1%, P=0.011; DFS: 83.3% vs. 80.6%, P=0.160), LDH >upper normal limit (OS: 88.2% vs. 72.9%, P=0.003; DFS: 86.8% vs.20.0%, P<0.001), IPI>0 (OS: 90.0% vs. 55.9%, P=0.007; DFS: 86.5% vs. 64.0%, P=0.034) and combination of CTx and RT (OS: 79.6% vs. 48.2%, P=0.025; DFS: 72.6% vs. 48.5%, P=0.038). Germinal center (GC) and non-GC phenotype were not predictors of outcome in localized primary DLBCL of the tonsil. Combination chemotherapy-treated patients with rituximab did not show a significantly better OS and DFS than the combination chemotherapy-treated patients without rituximab. On multivariate analysis; LDH >upper normal limit (DFS: hazard ratio [HR], 14.958; 95% CI, 2.474-90.432, P=0.003; OS: HR, 9.341; 95% CI, 1.635-53.361, P=0.012), and combination of CTx and RT (DFS: HR, 0.088: 95% CI, 0.009-0.834, P=0.034; OS: HR, 0.112; 95% CI, 0.014-0.918, P=0.041), retained statistical significance.
Summary
The DFS and OS rates were significantly better for patients receiving combination of CTx and RT. A combined treatment, consisting of CTx and RT results in a satisfactory outcome in patients with localized primary DLBCL of tonsil.
Keyword(s): Chemotherapy, Diffuse large B cell lymphoma, Radiotherapy
Session topic: Publication Only
{{ help_message }}
{{filter}}


