Department of hematology

Contributions
Type: Publication Only
Background
Individual lifestyle factors such as smoking and alcohol intake are common in the Western world and modify the risk of several cancer types, including non-Hodgkin lymphoma (NHL). However, less is known about the impact of these lifestyle factors on survival once the lymphoma has arisen.
Aims
To examine the prognostic impact of smoking and alcohol intake on overall survival (OS) in patients with newly diagnosed DLBCL treated with immunochemotherapy.
Methods
This retrospective study included adult patients with newly diagnosed DLBCL seen at the hematology centers of Aalborg (2003-2010), Holstebro (2006-2012), Odense (2006-2012), and Copenhagen (Rigshospitalet, 2010-2012). All patients had been treated with R-CHOP/CHOP-like regimens. Patient lists were obtained from the Danish Lymphoma registry (LYFO). The LYFO contains detailed information on a wide range of clinico-pathological features as well as complete follow-up data. Medical records were retrieved and reviewed for information on smoking habits, alcohol consumption, and comorbidities. Overall survival (OS) estimates were made using the Kaplan-Meier method. The impact of lifestyle and comorbidity on OS was evaluated with simple and multiple Cox models with inclusion of the standard international prognostic index (IPI) risk groups and comorbidities.
Results
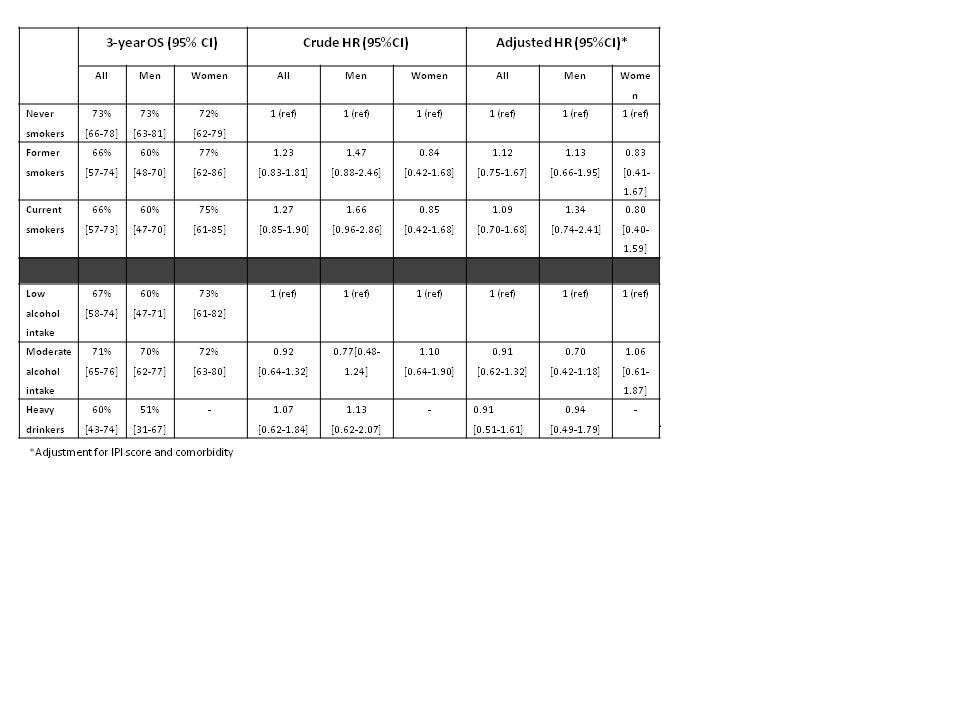
A total of 502 DLBCL patients had available information on smoking and alcohol intake and were included in the present study. Patients were categorized as low-risk (26%), low-intermediate (24%), intermediate-high (26%) and high risk (18%), according to the IPI. Never smokers accounted for 43% of the patients, former smokers 31%, and current smokers 26%. A low alcohol intake (<3 standard drinks per week) was noted in 33% of the patients, a moderate intake (3-14 standard drinks per week) in 55%, and heavy drinking (>14 standard drinks per week) in 11%. The Table shows the impact of lifestyle on outcome. In male patients, both current and former smoking were associated with a lower 3-year OS. Smoking habits did not influence survival in female patients. However, the associations between smoking and OS were attenuated after adjusting for comorbidities, which suggest that the effects of smoking were at least partially mediated by excess comorbidity in these patients. Participants with a moderate alcohol intake had the highest 3-years OS (71%), whereas heavy drinkers had the lowest 3-years OS (60%), but alcohol consumption did not have impact on survival in univariate or multivariate Cox analyses.
Summary
Overall, smoking habits and alcohol intake had no significant impact on the short term survival in this large cohort of uniformly treated DLBCL patients. However, current and former smoking were associated with a strong trend toward inferior OS, which is possibly mediated by excess comorbidity in this subset of patients.
Keyword(s): Diffuse large B cell lymphoma
Session topic: Publication Only
Type: Publication Only
Background
Individual lifestyle factors such as smoking and alcohol intake are common in the Western world and modify the risk of several cancer types, including non-Hodgkin lymphoma (NHL). However, less is known about the impact of these lifestyle factors on survival once the lymphoma has arisen.
Aims
To examine the prognostic impact of smoking and alcohol intake on overall survival (OS) in patients with newly diagnosed DLBCL treated with immunochemotherapy.
Methods
This retrospective study included adult patients with newly diagnosed DLBCL seen at the hematology centers of Aalborg (2003-2010), Holstebro (2006-2012), Odense (2006-2012), and Copenhagen (Rigshospitalet, 2010-2012). All patients had been treated with R-CHOP/CHOP-like regimens. Patient lists were obtained from the Danish Lymphoma registry (LYFO). The LYFO contains detailed information on a wide range of clinico-pathological features as well as complete follow-up data. Medical records were retrieved and reviewed for information on smoking habits, alcohol consumption, and comorbidities. Overall survival (OS) estimates were made using the Kaplan-Meier method. The impact of lifestyle and comorbidity on OS was evaluated with simple and multiple Cox models with inclusion of the standard international prognostic index (IPI) risk groups and comorbidities.
Results
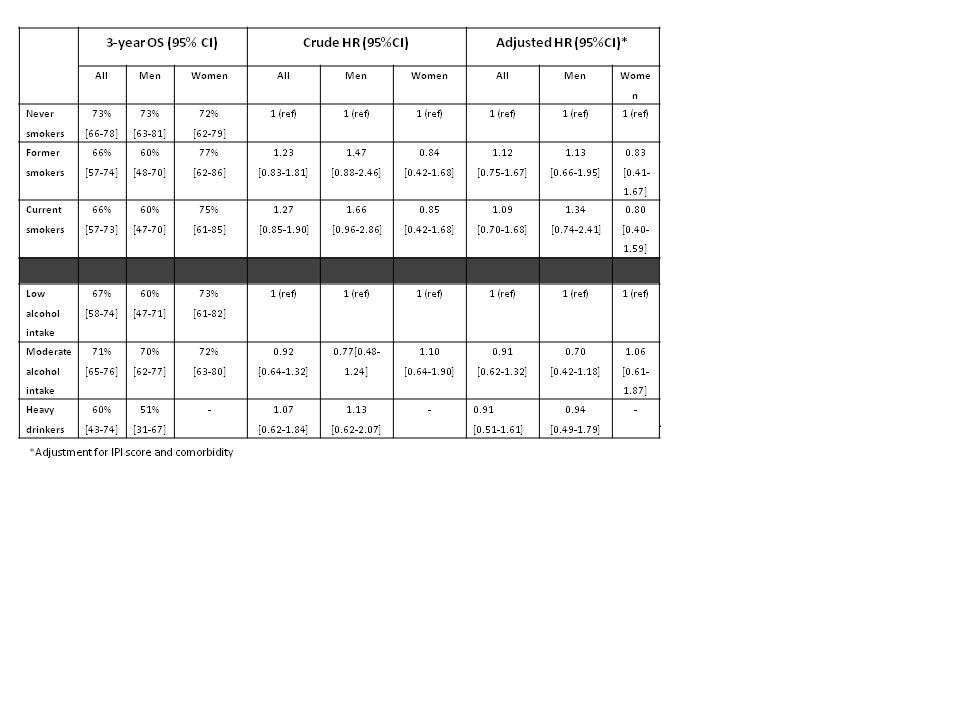
A total of 502 DLBCL patients had available information on smoking and alcohol intake and were included in the present study. Patients were categorized as low-risk (26%), low-intermediate (24%), intermediate-high (26%) and high risk (18%), according to the IPI. Never smokers accounted for 43% of the patients, former smokers 31%, and current smokers 26%. A low alcohol intake (<3 standard drinks per week) was noted in 33% of the patients, a moderate intake (3-14 standard drinks per week) in 55%, and heavy drinking (>14 standard drinks per week) in 11%. The Table shows the impact of lifestyle on outcome. In male patients, both current and former smoking were associated with a lower 3-year OS. Smoking habits did not influence survival in female patients. However, the associations between smoking and OS were attenuated after adjusting for comorbidities, which suggest that the effects of smoking were at least partially mediated by excess comorbidity in these patients. Participants with a moderate alcohol intake had the highest 3-years OS (71%), whereas heavy drinkers had the lowest 3-years OS (60%), but alcohol consumption did not have impact on survival in univariate or multivariate Cox analyses.
Summary
Overall, smoking habits and alcohol intake had no significant impact on the short term survival in this large cohort of uniformly treated DLBCL patients. However, current and former smoking were associated with a strong trend toward inferior OS, which is possibly mediated by excess comorbidity in this subset of patients.
Keyword(s): Diffuse large B cell lymphoma
Session topic: Publication Only


