
Contributions
Type: Publication Only
Background
High dose chemotherapy with autologous stem cell transplantation (ASCT) has been considered the standard of care for multiple myeloma patients and has been shown to increase both overall survival (OS) and progression free survival (PFS). However, the significance of initial treatment response and the significance of pretransplant disease status are not clear whether the depth of response influences the OS or PFS.
Aims
In this retrospective study we aimed to evaluate the significance of initial chemotherapy response and pretransplant disease status on PFS and OS.
Methods
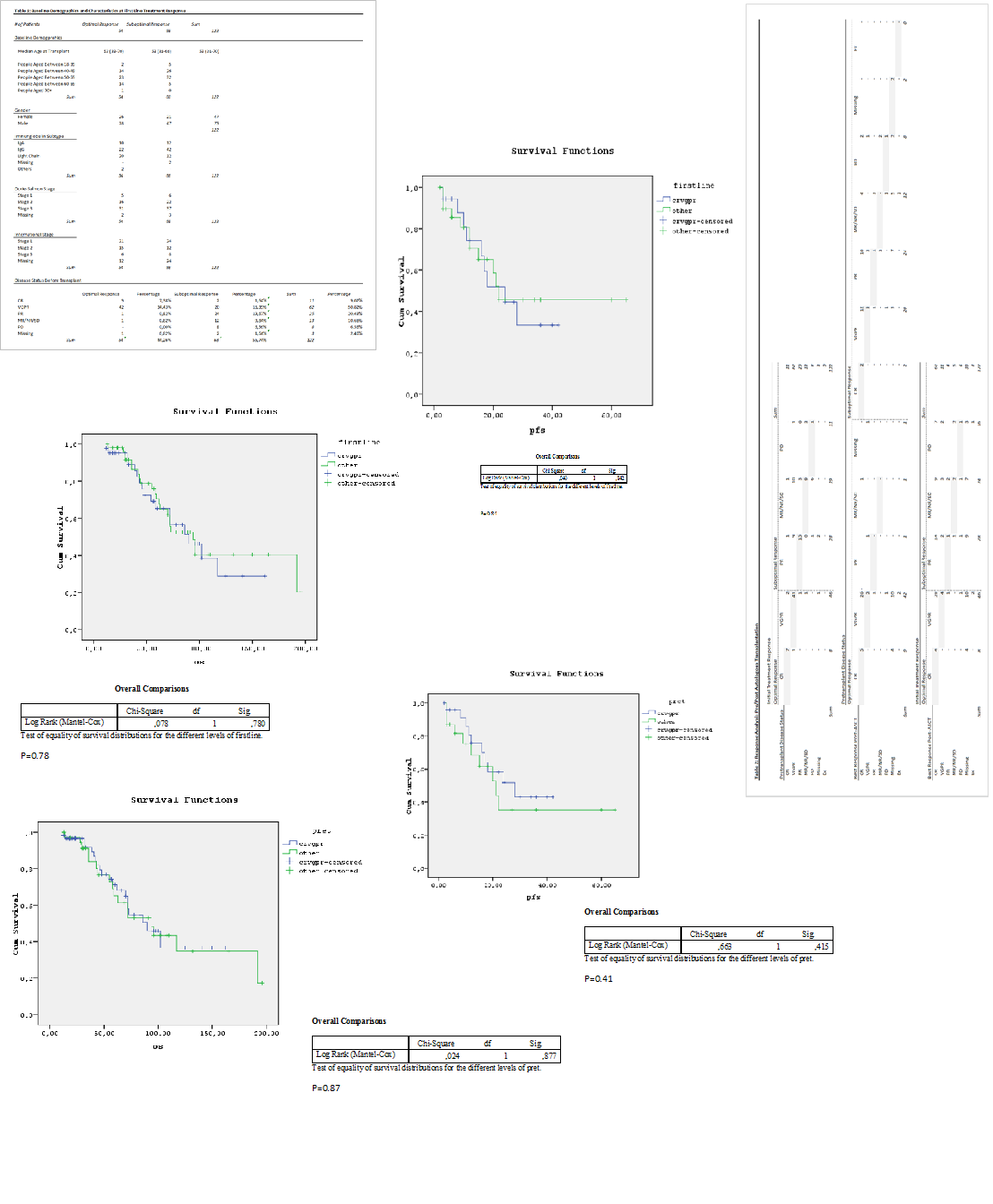
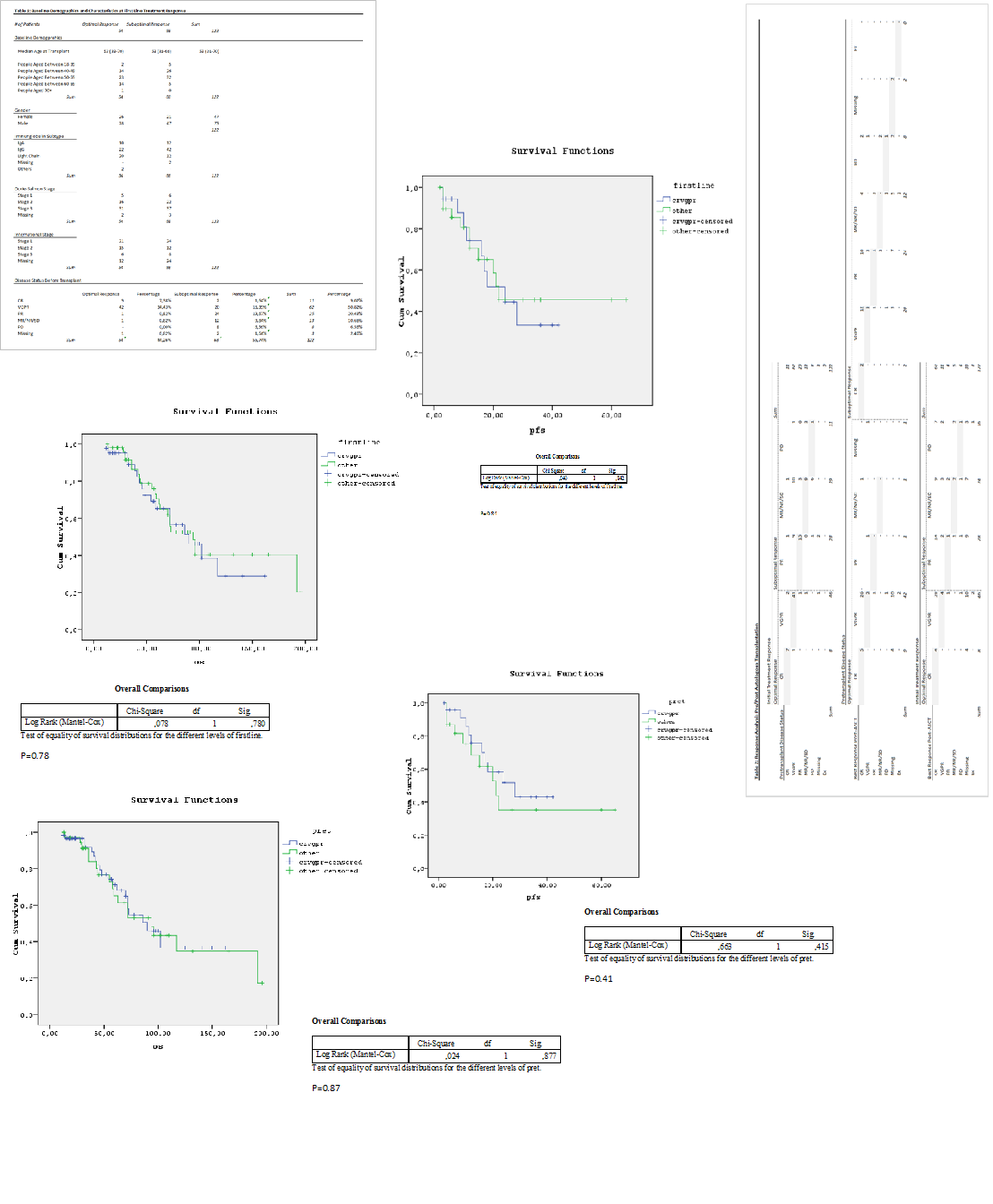
We identified 127 myeloma patients who underwent ASCT between 1997- 2014 at Istanbul University Cerrahpasa Medical Faculty. Five of them were excluded from the study due to missing first line response data. Remaining 122 were grouped according to the first line chemotherapy responses, as suboptimal and optimal. Standard International Myeloma Working Group criteria were used for classifying disease responses and defining progression of multiple myeloma. Suboptimal response to first line pretransplant therapy was defined as a failure to achieve at least a VGPR following the first line chemotherapy.
Demographic variables and disease related variables were given in Table 1. PFS and OS of patients in the 2 study cohorts were compared using Logrank test (Table 3)
Results
127 patients treated with high dose chemotherapy and ASCT between 1997-2014 were included in the study. Median follow up time is 56 months. Of these patients, 56% (n:68) failed to achieve an optimal response following the first line chemotherapy. Most of these patients received second line chemotherapy before proceeding to ASCT. Subsequent to additional chemotherapy, 37% (n:46) underwent ASCT. The overall survival of patients responded as CR or VGPR is 53 months.
Summary
In conclusion, for patients achieving less than a VGPR response following initial chemotherapy, additional chemotherapy improved depth of response, but was not associated with survival benefit. Furthermore we found no impact of initial treatment response on PFS and OS. This might be explained by the increased efficacy of new agents.
Keyword(s): Bone marrow transplant, Multiple myeloma
Session topic: Publication Only
Type: Publication Only
Background
High dose chemotherapy with autologous stem cell transplantation (ASCT) has been considered the standard of care for multiple myeloma patients and has been shown to increase both overall survival (OS) and progression free survival (PFS). However, the significance of initial treatment response and the significance of pretransplant disease status are not clear whether the depth of response influences the OS or PFS.
Aims
In this retrospective study we aimed to evaluate the significance of initial chemotherapy response and pretransplant disease status on PFS and OS.
Methods
We identified 127 myeloma patients who underwent ASCT between 1997- 2014 at Istanbul University Cerrahpasa Medical Faculty. Five of them were excluded from the study due to missing first line response data. Remaining 122 were grouped according to the first line chemotherapy responses, as suboptimal and optimal. Standard International Myeloma Working Group criteria were used for classifying disease responses and defining progression of multiple myeloma. Suboptimal response to first line pretransplant therapy was defined as a failure to achieve at least a VGPR following the first line chemotherapy.
Demographic variables and disease related variables were given in Table 1. PFS and OS of patients in the 2 study cohorts were compared using Logrank test (Table 3)
Results
127 patients treated with high dose chemotherapy and ASCT between 1997-2014 were included in the study. Median follow up time is 56 months. Of these patients, 56% (n:68) failed to achieve an optimal response following the first line chemotherapy. Most of these patients received second line chemotherapy before proceeding to ASCT. Subsequent to additional chemotherapy, 37% (n:46) underwent ASCT. The overall survival of patients responded as CR or VGPR is 53 months.
Summary
In conclusion, for patients achieving less than a VGPR response following initial chemotherapy, additional chemotherapy improved depth of response, but was not associated with survival benefit. Furthermore we found no impact of initial treatment response on PFS and OS. This might be explained by the increased efficacy of new agents.
Keyword(s): Bone marrow transplant, Multiple myeloma
Session topic: Publication Only


