SURVIVAL BENEFIT OF HEMATOPOIETIC STEM-CELL TRANSPLANTION FOR PTCLS: A RETROSPECTIVE COMPARISON STUDY BETWEEN CONVENTIONAL CHEMOTHERAPY AND STEM CELL TRANSPLANTATION FOR PTCLS FROM A CHINESE CENTER
(Abstract release date: 05/21/15)
EHA Library. Huang H. 06/12/15; 102861; PB1673
Disclosure(s): The First Affiliated Hospital of Soochow Universityhematology

Dr. Haiwen Huang
Contributions
Contributions
Abstract
Abstract: PB1673
Type: Publication Only
Background
Peripheral T-cell lymphomas (PTCLs) are rare malignancies with poor outcome after conventional chemotherapy. The role of stem cell transplantion in the treatment of PTCLs is still unclear.
Aims
Here, we present the result of a comparison study between conventional chemotherapy and stem cell transplantation for PTCLs in our centre.
Methods
From July 2004 to July 2014, 104 cases were analyzed retrospectively, including age, IPI score and morbid state before transplantion. 52 patients underwent HSCT including angioimmunoblastic T-cell lmphoma(n=15), anaplastic large cell lymphoma(n=14), PTCL not specified(n=12), NK/T cell lymphoma(n=11). In this group, 43 patients were IPI≥3-4). Thirty-three patients(63.5%) received autologous stem-cell transplantion (autoSCT) and nineteen patients (36.5%) received allogeneic stem-cell transplantion (allo-SCT). Before stem-cell transplantation, 43 Patients were in complete remission (CR), 2 patients were in partial remission (PR), 7 patients were not-remission(NR). In conventional chemotherapy group, 52 patients (median age, 49.5 years, IPI≥3-4: 40 patients ) only received conventional chemotherapy. Primary outcomes of progression-free survival (PFS), and overall survival (OS) rates were estimated by using the Kaplan-Meier method.
Results
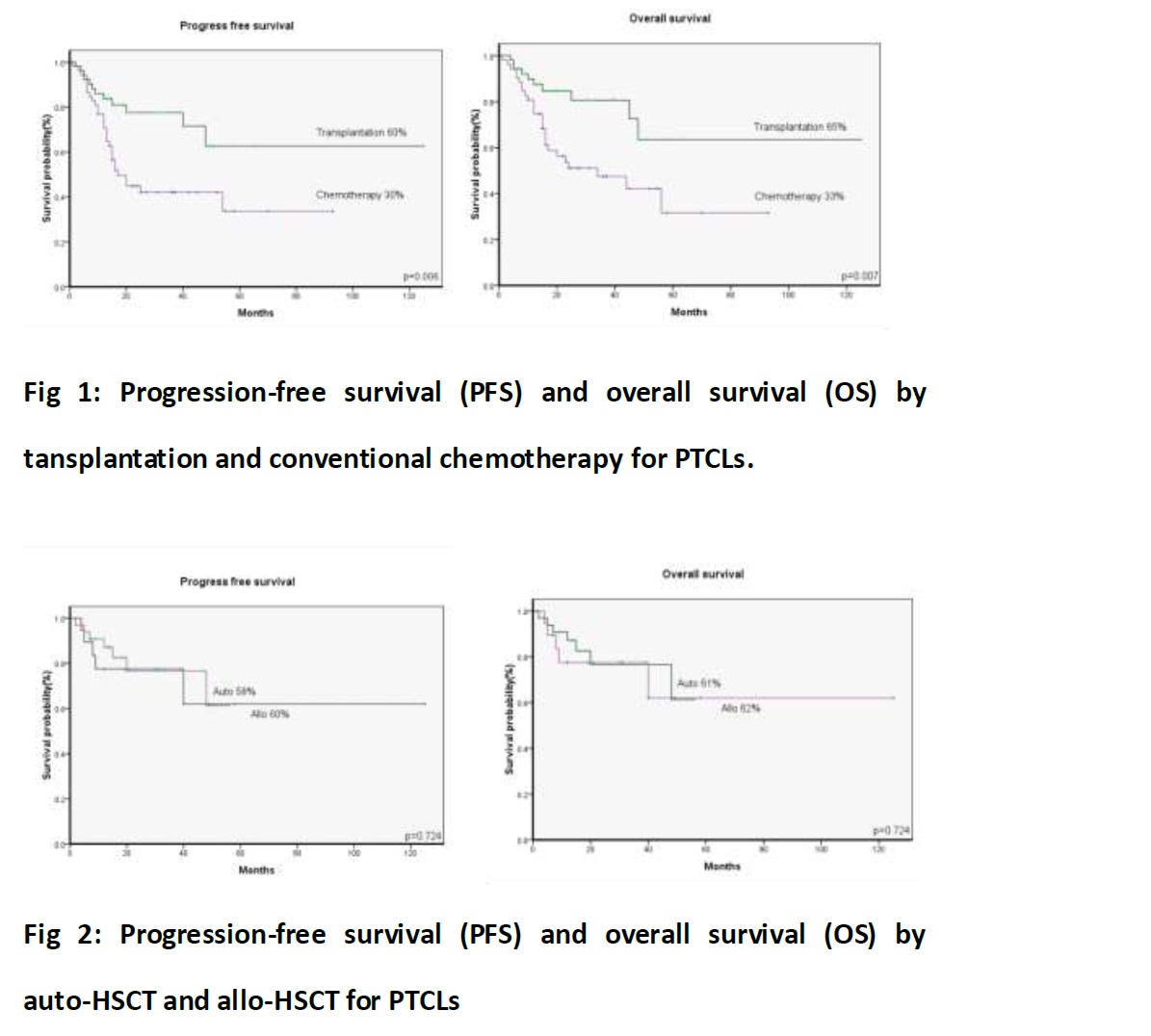
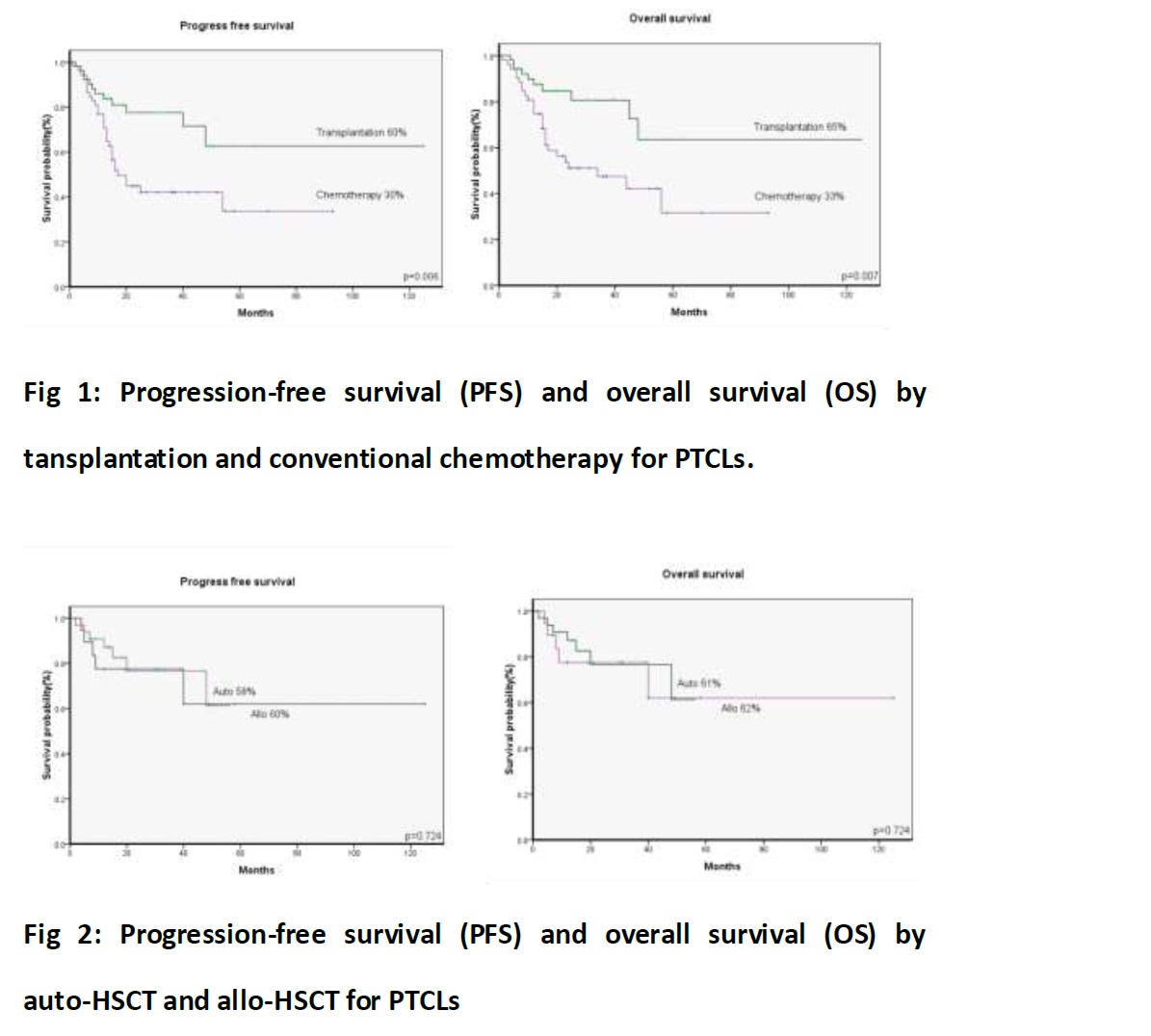
After a median follow-up of 23.5 months, K-M analysis showed that the 5-year PFS for HSCT and chemotherapy were 60% and 30%(p=0.006), the 5-year OS were 65% and 33% (p=0.007)(Fig 1), respectively. These results suggested that frontline stem cell transplantation for high-risk PTCLs may improve treatment outcome. The 5-year PFS for autoHSCT and alloHSCT were 60% and 58%(p=0.074) . The 5-year OS were 62% and 61% (p=0.074) (Fig 2). There were no significant survival differences between the auto-HSCT and allo-HSCT.
Summary
The results of this retrospective study suggest that HSCT have great advantange copared to conventional chemtherapy on long-term survival in peripheral T-cell lymphomas. However, the resullt of auto-HSCT and allo-HSCT seems to have no difference. Therefore, autoHSCT should be considered to be the first -line therapy in peripheral T-cell lymphomas, especially for those patients with high risk factors.
Keyword(s): Peripheral T-cell lymphoma, Transplant
Session topic: Publication Only
Type: Publication Only
Background
Peripheral T-cell lymphomas (PTCLs) are rare malignancies with poor outcome after conventional chemotherapy. The role of stem cell transplantion in the treatment of PTCLs is still unclear.
Aims
Here, we present the result of a comparison study between conventional chemotherapy and stem cell transplantation for PTCLs in our centre.
Methods
From July 2004 to July 2014, 104 cases were analyzed retrospectively, including age, IPI score and morbid state before transplantion. 52 patients underwent HSCT including angioimmunoblastic T-cell lmphoma(n=15), anaplastic large cell lymphoma(n=14), PTCL not specified(n=12), NK/T cell lymphoma(n=11). In this group, 43 patients were IPI≥3-4). Thirty-three patients(63.5%) received autologous stem-cell transplantion (autoSCT) and nineteen patients (36.5%) received allogeneic stem-cell transplantion (allo-SCT). Before stem-cell transplantation, 43 Patients were in complete remission (CR), 2 patients were in partial remission (PR), 7 patients were not-remission(NR). In conventional chemotherapy group, 52 patients (median age, 49.5 years, IPI≥3-4: 40 patients ) only received conventional chemotherapy. Primary outcomes of progression-free survival (PFS), and overall survival (OS) rates were estimated by using the Kaplan-Meier method.
Results
After a median follow-up of 23.5 months, K-M analysis showed that the 5-year PFS for HSCT and chemotherapy were 60% and 30%(p=0.006), the 5-year OS were 65% and 33% (p=0.007)(Fig 1), respectively. These results suggested that frontline stem cell transplantation for high-risk PTCLs may improve treatment outcome. The 5-year PFS for autoHSCT and alloHSCT were 60% and 58%(p=0.074) . The 5-year OS were 62% and 61% (p=0.074) (Fig 2). There were no significant survival differences between the auto-HSCT and allo-HSCT.
Summary
The results of this retrospective study suggest that HSCT have great advantange copared to conventional chemtherapy on long-term survival in peripheral T-cell lymphomas. However, the resullt of auto-HSCT and allo-HSCT seems to have no difference. Therefore, autoHSCT should be considered to be the first -line therapy in peripheral T-cell lymphomas, especially for those patients with high risk factors.
Keyword(s): Peripheral T-cell lymphoma, Transplant
Session topic: Publication Only
Abstract: PB1673
Type: Publication Only
Background
Peripheral T-cell lymphomas (PTCLs) are rare malignancies with poor outcome after conventional chemotherapy. The role of stem cell transplantion in the treatment of PTCLs is still unclear.
Aims
Here, we present the result of a comparison study between conventional chemotherapy and stem cell transplantation for PTCLs in our centre.
Methods
From July 2004 to July 2014, 104 cases were analyzed retrospectively, including age, IPI score and morbid state before transplantion. 52 patients underwent HSCT including angioimmunoblastic T-cell lmphoma(n=15), anaplastic large cell lymphoma(n=14), PTCL not specified(n=12), NK/T cell lymphoma(n=11). In this group, 43 patients were IPI≥3-4). Thirty-three patients(63.5%) received autologous stem-cell transplantion (autoSCT) and nineteen patients (36.5%) received allogeneic stem-cell transplantion (allo-SCT). Before stem-cell transplantation, 43 Patients were in complete remission (CR), 2 patients were in partial remission (PR), 7 patients were not-remission(NR). In conventional chemotherapy group, 52 patients (median age, 49.5 years, IPI≥3-4: 40 patients ) only received conventional chemotherapy. Primary outcomes of progression-free survival (PFS), and overall survival (OS) rates were estimated by using the Kaplan-Meier method.
Results
After a median follow-up of 23.5 months, K-M analysis showed that the 5-year PFS for HSCT and chemotherapy were 60% and 30%(p=0.006), the 5-year OS were 65% and 33% (p=0.007)(Fig 1), respectively. These results suggested that frontline stem cell transplantation for high-risk PTCLs may improve treatment outcome. The 5-year PFS for autoHSCT and alloHSCT were 60% and 58%(p=0.074) . The 5-year OS were 62% and 61% (p=0.074) (Fig 2). There were no significant survival differences between the auto-HSCT and allo-HSCT.
Summary
The results of this retrospective study suggest that HSCT have great advantange copared to conventional chemtherapy on long-term survival in peripheral T-cell lymphomas. However, the resullt of auto-HSCT and allo-HSCT seems to have no difference. Therefore, autoHSCT should be considered to be the first -line therapy in peripheral T-cell lymphomas, especially for those patients with high risk factors.
Keyword(s): Peripheral T-cell lymphoma, Transplant
Session topic: Publication Only
Type: Publication Only
Background
Peripheral T-cell lymphomas (PTCLs) are rare malignancies with poor outcome after conventional chemotherapy. The role of stem cell transplantion in the treatment of PTCLs is still unclear.
Aims
Here, we present the result of a comparison study between conventional chemotherapy and stem cell transplantation for PTCLs in our centre.
Methods
From July 2004 to July 2014, 104 cases were analyzed retrospectively, including age, IPI score and morbid state before transplantion. 52 patients underwent HSCT including angioimmunoblastic T-cell lmphoma(n=15), anaplastic large cell lymphoma(n=14), PTCL not specified(n=12), NK/T cell lymphoma(n=11). In this group, 43 patients were IPI≥3-4). Thirty-three patients(63.5%) received autologous stem-cell transplantion (autoSCT) and nineteen patients (36.5%) received allogeneic stem-cell transplantion (allo-SCT). Before stem-cell transplantation, 43 Patients were in complete remission (CR), 2 patients were in partial remission (PR), 7 patients were not-remission(NR). In conventional chemotherapy group, 52 patients (median age, 49.5 years, IPI≥3-4: 40 patients ) only received conventional chemotherapy. Primary outcomes of progression-free survival (PFS), and overall survival (OS) rates were estimated by using the Kaplan-Meier method.
Results
After a median follow-up of 23.5 months, K-M analysis showed that the 5-year PFS for HSCT and chemotherapy were 60% and 30%(p=0.006), the 5-year OS were 65% and 33% (p=0.007)(Fig 1), respectively. These results suggested that frontline stem cell transplantation for high-risk PTCLs may improve treatment outcome. The 5-year PFS for autoHSCT and alloHSCT were 60% and 58%(p=0.074) . The 5-year OS were 62% and 61% (p=0.074) (Fig 2). There were no significant survival differences between the auto-HSCT and allo-HSCT.
Summary
The results of this retrospective study suggest that HSCT have great advantange copared to conventional chemtherapy on long-term survival in peripheral T-cell lymphomas. However, the resullt of auto-HSCT and allo-HSCT seems to have no difference. Therefore, autoHSCT should be considered to be the first -line therapy in peripheral T-cell lymphomas, especially for those patients with high risk factors.
Keyword(s): Peripheral T-cell lymphoma, Transplant
Session topic: Publication Only
{{ help_message }}
{{filter}}


