Contributions
Type: Publication Only
Background
Thrombocytosis is a common feature in chronic myeloproliferative disorders. The incidence of thrombocytosis in CML is reported to be around 30 to 50%. Extreme thrombocytosis defined as a platelet (PLT) count > 1.000 x 109/l is uncommon in CML as well as isolated thrombocytosis.
Aims
Our aim is to study the clinical management and the therapeutic response of CML with extreme thrombocytosis.
Methods
From January 2001 to January 2015, 1314 patients affected by CML were followed in 15 different Italian hematological centers. We diagnosed 78 CML with extreme thrombocytosis at onset (5.9%); we conducted the study on 70 pts who have at least 6 months of follow-up and were in chronic phase; 2 pts in blast phase and in accelerated phase were excluded from the analysis.
Results
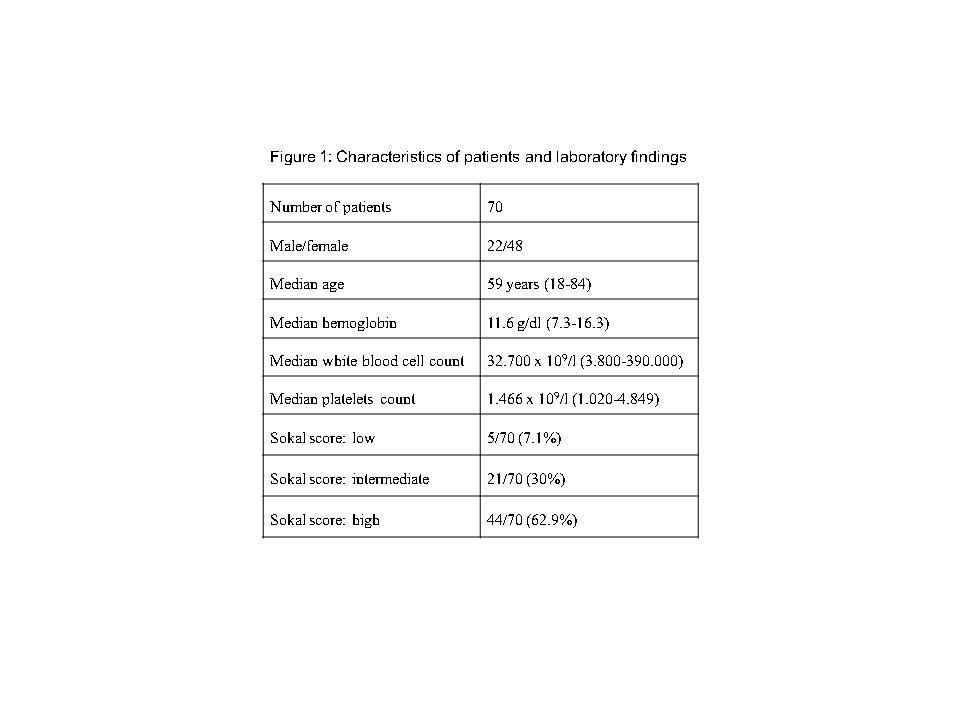
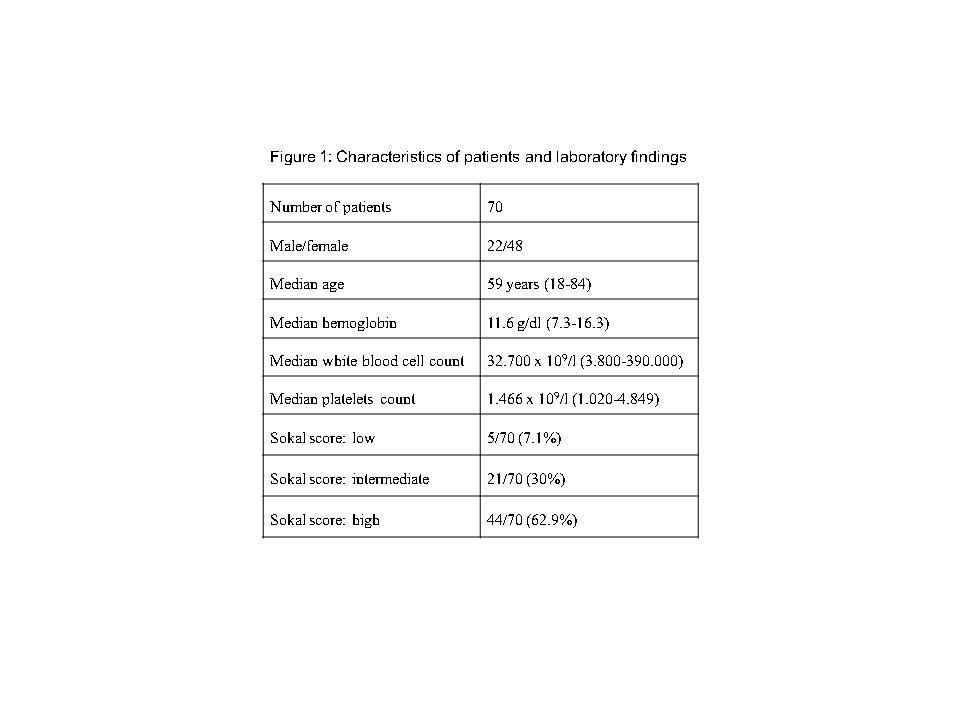
Our patients were 48 females and 22 males with a median age of 59 years (range 18-84). At diagnosis, median hemoglobin level was 11.6 g/dl, median WBC 32.7 x 109/l and PLT count 1.466 x 109/l. The Sokal score was high in 44 (62.9%), intermediate in 21 (30%) and low in 5 (7.1%). According to Hasford score 47.5% pts resulted high, 30.5% intermediate, 22% high; Eutos score available in 48/70 pts was high in 13 (27.1%) and low in 35 (72.9%). Pts’ characteristics are summarized in Figure 1.
PCR analysis showed the presence of p210 in all cases and the absence of JAK2 V617F mutation in 28 out of 30 pts (42.9% of all the pts) who performed the test.
At diagnosis we registered 5 thrombotic/hemorrhagic episodes: 1 superficial thrombosis, 1 subarachnoid hemorrhage, 1 metrorrhagia, 1 epistaxis and 1 purpura. None of the two JAK2 positive patients showed thrombotic/hemorrhagic episodes.
All but six pts received initial treatment with hydroxyurea and allopurinol. One patient underwent PLT apheresis. PLT count was generally unresponsive to initial treatment. Upfront treatment was imatinib in 53 pts, nilotinib in 11 pts and dasatinib in 6 pts. PLT count normalization was rapidly achieved after introduction of TKIs. Hematological response was reached at a median of 1 month, complete cytogenetic response after a median of 3 months (range 3-36) in 62/65 evaluable pts, and major molecular response in 53 out of 64 evaluable pts after a median of 9 months (range 3-101).
Of the 53 pts who started imatinib 7 pts shifted to nilotinib for resistance (3 primary and 4 secondary), 3 to dasatinib for primary resistance, 1 to ponatinib for primary resistance and 2 pts are not on TKI at this time for intolerance. Four of these pts dead for causes independent from CML (1 pt for myocardial infarction, 1 pt for GVHD post-transplantation and 2 pts for second tumor at 3, 9, 38 and 147 months respectively) and 3 pts were lost during follow-up. Three patients of the 11 who started nilotinib stopped treatment with TKIs for resistance or intolerance, 1 shifted to dasatinib for secondary resistance.
Sixty-three patients (90%) are alive, 58 of them on TKIs (33 imatinib, 14 nilotinib, 10 dasatinib, 1 ponatinib) at a median follow up of 65 months (range 7-168).
Summary
The prevalence of extreme thrombocytosis in CML is 5.9% in a large multicenter observational study. Cytoreduction with hydroxyurea was not able to achieve normalization of PLT count, however pts with extreme thrombocytosis were easily and rapidly managed by TKIs. CML pts with extreme thrombocytosis resulted similar to the CML population considering the response to TKIs and low number of thrombotic/hemorrhagic complications. Patients on at least major molecular response are 48 out of 55 evaluable (87.3%) at a median follow-up of 65 months.
Keyword(s): Chronic myeloid leukemia, Thrombocytosis, Tyrosine kinase inhibitor
Type: Publication Only
Background
Thrombocytosis is a common feature in chronic myeloproliferative disorders. The incidence of thrombocytosis in CML is reported to be around 30 to 50%. Extreme thrombocytosis defined as a platelet (PLT) count > 1.000 x 109/l is uncommon in CML as well as isolated thrombocytosis.
Aims
Our aim is to study the clinical management and the therapeutic response of CML with extreme thrombocytosis.
Methods
From January 2001 to January 2015, 1314 patients affected by CML were followed in 15 different Italian hematological centers. We diagnosed 78 CML with extreme thrombocytosis at onset (5.9%); we conducted the study on 70 pts who have at least 6 months of follow-up and were in chronic phase; 2 pts in blast phase and in accelerated phase were excluded from the analysis.
Results
Our patients were 48 females and 22 males with a median age of 59 years (range 18-84). At diagnosis, median hemoglobin level was 11.6 g/dl, median WBC 32.7 x 109/l and PLT count 1.466 x 109/l. The Sokal score was high in 44 (62.9%), intermediate in 21 (30%) and low in 5 (7.1%). According to Hasford score 47.5% pts resulted high, 30.5% intermediate, 22% high; Eutos score available in 48/70 pts was high in 13 (27.1%) and low in 35 (72.9%). Pts’ characteristics are summarized in Figure 1.
PCR analysis showed the presence of p210 in all cases and the absence of JAK2 V617F mutation in 28 out of 30 pts (42.9% of all the pts) who performed the test.
At diagnosis we registered 5 thrombotic/hemorrhagic episodes: 1 superficial thrombosis, 1 subarachnoid hemorrhage, 1 metrorrhagia, 1 epistaxis and 1 purpura. None of the two JAK2 positive patients showed thrombotic/hemorrhagic episodes.
All but six pts received initial treatment with hydroxyurea and allopurinol. One patient underwent PLT apheresis. PLT count was generally unresponsive to initial treatment. Upfront treatment was imatinib in 53 pts, nilotinib in 11 pts and dasatinib in 6 pts. PLT count normalization was rapidly achieved after introduction of TKIs. Hematological response was reached at a median of 1 month, complete cytogenetic response after a median of 3 months (range 3-36) in 62/65 evaluable pts, and major molecular response in 53 out of 64 evaluable pts after a median of 9 months (range 3-101).
Of the 53 pts who started imatinib 7 pts shifted to nilotinib for resistance (3 primary and 4 secondary), 3 to dasatinib for primary resistance, 1 to ponatinib for primary resistance and 2 pts are not on TKI at this time for intolerance. Four of these pts dead for causes independent from CML (1 pt for myocardial infarction, 1 pt for GVHD post-transplantation and 2 pts for second tumor at 3, 9, 38 and 147 months respectively) and 3 pts were lost during follow-up. Three patients of the 11 who started nilotinib stopped treatment with TKIs for resistance or intolerance, 1 shifted to dasatinib for secondary resistance.
Sixty-three patients (90%) are alive, 58 of them on TKIs (33 imatinib, 14 nilotinib, 10 dasatinib, 1 ponatinib) at a median follow up of 65 months (range 7-168).
Summary
The prevalence of extreme thrombocytosis in CML is 5.9% in a large multicenter observational study. Cytoreduction with hydroxyurea was not able to achieve normalization of PLT count, however pts with extreme thrombocytosis were easily and rapidly managed by TKIs. CML pts with extreme thrombocytosis resulted similar to the CML population considering the response to TKIs and low number of thrombotic/hemorrhagic complications. Patients on at least major molecular response are 48 out of 55 evaluable (87.3%) at a median follow-up of 65 months.
Keyword(s): Chronic myeloid leukemia, Thrombocytosis, Tyrosine kinase inhibitor