hematology

Contributions
Type: Publication Only
Background
Despite the advent of newer targeted and immune therapies, allogeneic hematopoietic cell transplantation (HCT) still offers an advantage in terms of disease free survival, overall survival and quality of life in appropriate settings.
Aims
Several studies have elucidated the heterogeneity in HCT practice among individual physicians, transplant centers and different countries. In our institution, we conducted a retrospective analysis describing and evaluating the outcome of patients for whom an allogeneic HCT was discussed or planned.
Methods
From 2007 till the end of 2014, an HLA typing was done for 156 patients treated for different hematological malignancies at Centre Rene Huguenin/ Institut Curie, France. We reviewed the files of these patients for the type of malignancy, the reason why HLA typing was done, the major barriers to allogeneic HCT and the different outcomes.
Results
Among the 156 patients, 27.5% had acute myeloid leukemia, 5.8% acute lymphoblastic leukemia, 0.6% biphenotypic leukemia, 1.9% plasmacytic leukemia, 15.4% multiple myeloma, 7.1% hodgkin lymphoma, 16.1% non hodgkin lymphoma, 7.7% chronic lymphocytic leukemia, 12.8% myelodysplastic syndrome, 5.1% myeloproliferative neoplasms.
Of these, 14.1% were typed before complete risk stratification of the disease, 37.2% for the presence of high risk factors (e.g karyotype, molecular markers, …), 17.3% because their disease was refractory to primary treatment or had an early relapse, 30.8% for late and multiple relapses, and 0.6% upon patient’s request.
Fifty nine patients or 37.8% underwent allogeneic hematopoietic cell transplantation and 7.1% are currently being evaluated by the committee. The median age of the patients undergoing allogeneic HCT was 53 years (19-67years) and those for whom an HLA typing was done was 57 years (19-72years). Median time from HLA typing to HCT was 7 months ranging from 1 to 14 months.
For the remaining patients, in 31.4% of the cases, allogeneic HCT was finally not indicated due to favorable prognosis, 25.6% didn't have a matched donor, 15.1% were ineligible because of refractory/resistant disease and 15.1% were also ineligible because of high risk comorbidities. In 10.5% of cases, the patients refused to undergo HCT and 2.3% were lost to follow up.
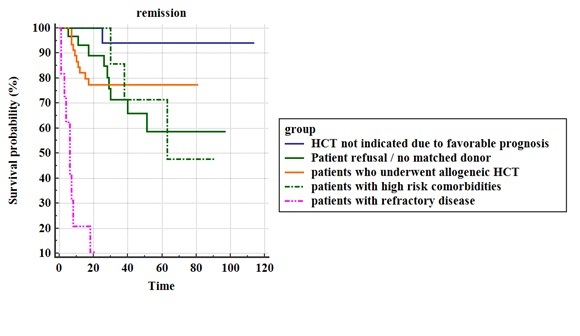
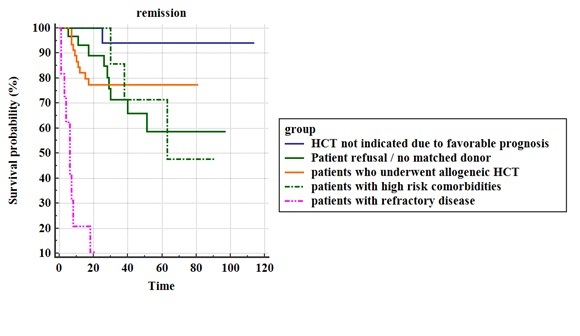
In terms of outcome, the patients with no indication to HCT due to a favorable prognosis had a significantly better survival than all others. Patients ineligible to HCT with a refractory/resistant disease had the poorer outcome. The group of patients undergoing allogeneic HCT had a lower relapse rates (10.1%) compared to those who didn't have a matched donor or who refused transplantation (22.5%) but there was no significant difference in survival between these groups possibly due to a transplant related mortality of 20.4%.
Summary
In patients for whom HCT was discussed in our institution, a favorable prognosis was the main cause for not undergoing HCT. The major barriers were lack of matched donors, patient's refusal and significant comorbidities. Our results show that current risk stratification of the hematological malignancies correlates well with the patients outcome. Clear criteria for allogeneic HCT are still lacking especially with the advent of new targeted therapies and the persistence of a significant transplant related mortality and morbidity.
Keyword(s): Allogeneic hematopoietic stem cell transplant, HLA, Outcome
Session topic: Publication Only
Type: Publication Only
Background
Despite the advent of newer targeted and immune therapies, allogeneic hematopoietic cell transplantation (HCT) still offers an advantage in terms of disease free survival, overall survival and quality of life in appropriate settings.
Aims
Several studies have elucidated the heterogeneity in HCT practice among individual physicians, transplant centers and different countries. In our institution, we conducted a retrospective analysis describing and evaluating the outcome of patients for whom an allogeneic HCT was discussed or planned.
Methods
From 2007 till the end of 2014, an HLA typing was done for 156 patients treated for different hematological malignancies at Centre Rene Huguenin/ Institut Curie, France. We reviewed the files of these patients for the type of malignancy, the reason why HLA typing was done, the major barriers to allogeneic HCT and the different outcomes.
Results
Among the 156 patients, 27.5% had acute myeloid leukemia, 5.8% acute lymphoblastic leukemia, 0.6% biphenotypic leukemia, 1.9% plasmacytic leukemia, 15.4% multiple myeloma, 7.1% hodgkin lymphoma, 16.1% non hodgkin lymphoma, 7.7% chronic lymphocytic leukemia, 12.8% myelodysplastic syndrome, 5.1% myeloproliferative neoplasms.
Of these, 14.1% were typed before complete risk stratification of the disease, 37.2% for the presence of high risk factors (e.g karyotype, molecular markers, …), 17.3% because their disease was refractory to primary treatment or had an early relapse, 30.8% for late and multiple relapses, and 0.6% upon patient’s request.
Fifty nine patients or 37.8% underwent allogeneic hematopoietic cell transplantation and 7.1% are currently being evaluated by the committee. The median age of the patients undergoing allogeneic HCT was 53 years (19-67years) and those for whom an HLA typing was done was 57 years (19-72years). Median time from HLA typing to HCT was 7 months ranging from 1 to 14 months.
For the remaining patients, in 31.4% of the cases, allogeneic HCT was finally not indicated due to favorable prognosis, 25.6% didn't have a matched donor, 15.1% were ineligible because of refractory/resistant disease and 15.1% were also ineligible because of high risk comorbidities. In 10.5% of cases, the patients refused to undergo HCT and 2.3% were lost to follow up.
In terms of outcome, the patients with no indication to HCT due to a favorable prognosis had a significantly better survival than all others. Patients ineligible to HCT with a refractory/resistant disease had the poorer outcome. The group of patients undergoing allogeneic HCT had a lower relapse rates (10.1%) compared to those who didn't have a matched donor or who refused transplantation (22.5%) but there was no significant difference in survival between these groups possibly due to a transplant related mortality of 20.4%.
Summary
In patients for whom HCT was discussed in our institution, a favorable prognosis was the main cause for not undergoing HCT. The major barriers were lack of matched donors, patient's refusal and significant comorbidities. Our results show that current risk stratification of the hematological malignancies correlates well with the patients outcome. Clear criteria for allogeneic HCT are still lacking especially with the advent of new targeted therapies and the persistence of a significant transplant related mortality and morbidity.
Keyword(s): Allogeneic hematopoietic stem cell transplant, HLA, Outcome
Session topic: Publication Only


