
Contributions
Type: Publication Only
Background
Autoimmune haemolytic anaemia (AIHA), usually classified as warm (WAIHA), cold (CAD), mixed, and atypical forms, is a greatly heterogeneous condition both in terms of clinical presentation and response to treatment, varying from mild/fully compensated to very severe, life-threatening and fatal.
Aims
To describe acute and very severe cases of AIHA who displayed multi-drug refractoriness and related complications.
Methods
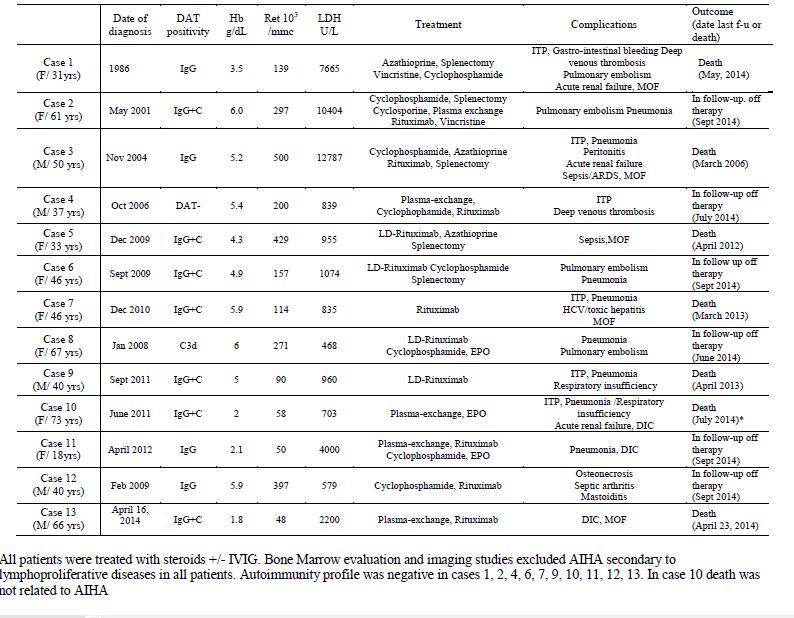
13 consecutive patients were identified among 157 primary AIHA followed from 1996 to 2014 at our institution. Patients were selected on the basis of very severe clinical presentation (Hb<6 g/dL, 51 cases) and requirement of at least 3 lines of therapy [steroids +/- IVIG, splenectomy, various immunesuppressants, plasma-exchange (PEX) and erythropoietin, 13/51].
Results
Table 1 shows the clinical characteristics of patients: 7 cases were direct antiglobulin test (DAT) positive with IgG+C antisera, 4 with IgG, and 1 with C; 1 case was DAT negative. All displayed marked intravascular haemolysis, 8 inadequate reticulocytosis, and 6 immune thrombocytopenia. Thrombotic events occurred in 8 patients (of whom 4 pulmonary embolism and 3 disseminated intravascular haemolysis) and acute renal failure in 3. All patients (but a Jehovah witness) received transfusions and steroids +/- intravenous immunoglobulins, 11 rituximab, 9 immunosuppressants, 5 PEX, 3 erythropoietin and 5 underwent splenectomy. Seven cases (54%) were fatal. In most cases death was due to infections and multiple organ failure, and was related with multi-treatment, particularly splenectomy, and with concomitant thrombocytopenia. Thrombotic complications were not fatal, and occurred more frequently in splenectomised cases.
Summary
The challenging AIHA cases described showed a greatly unpredictable clinical course. Evans syndrome and previous splenectomy, particularly when performed after multiple immunosuppressive therapies, were associated with poor prognosis. Rituximab, when promptly administered, was effective in solving the clinical emergency in most cases unresponsive to steroids and transfusions. Plasma exchange and erythropoietin were valuable options. Above all, in very severe AIHAs a scrupulous and continuous attention by experienced clinicians is required in order to avoid a delay in potentially life-saving strategies.
Keyword(s): Autoimmune hemolytic anemia (AIHA)
Session topic: Publication Only
Type: Publication Only
Background
Autoimmune haemolytic anaemia (AIHA), usually classified as warm (WAIHA), cold (CAD), mixed, and atypical forms, is a greatly heterogeneous condition both in terms of clinical presentation and response to treatment, varying from mild/fully compensated to very severe, life-threatening and fatal.
Aims
To describe acute and very severe cases of AIHA who displayed multi-drug refractoriness and related complications.
Methods
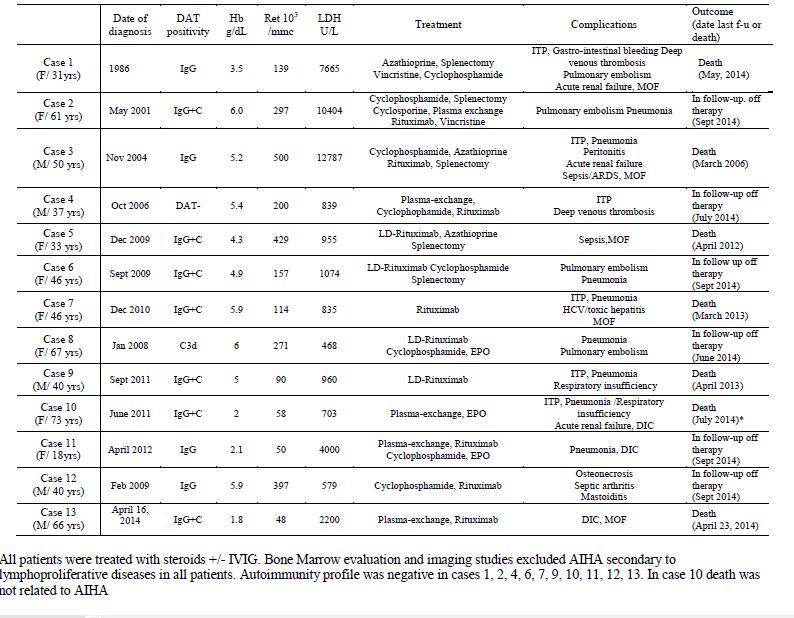
13 consecutive patients were identified among 157 primary AIHA followed from 1996 to 2014 at our institution. Patients were selected on the basis of very severe clinical presentation (Hb<6 g/dL, 51 cases) and requirement of at least 3 lines of therapy [steroids +/- IVIG, splenectomy, various immunesuppressants, plasma-exchange (PEX) and erythropoietin, 13/51].
Results
Table 1 shows the clinical characteristics of patients: 7 cases were direct antiglobulin test (DAT) positive with IgG+C antisera, 4 with IgG, and 1 with C; 1 case was DAT negative. All displayed marked intravascular haemolysis, 8 inadequate reticulocytosis, and 6 immune thrombocytopenia. Thrombotic events occurred in 8 patients (of whom 4 pulmonary embolism and 3 disseminated intravascular haemolysis) and acute renal failure in 3. All patients (but a Jehovah witness) received transfusions and steroids +/- intravenous immunoglobulins, 11 rituximab, 9 immunosuppressants, 5 PEX, 3 erythropoietin and 5 underwent splenectomy. Seven cases (54%) were fatal. In most cases death was due to infections and multiple organ failure, and was related with multi-treatment, particularly splenectomy, and with concomitant thrombocytopenia. Thrombotic complications were not fatal, and occurred more frequently in splenectomised cases.
Summary
The challenging AIHA cases described showed a greatly unpredictable clinical course. Evans syndrome and previous splenectomy, particularly when performed after multiple immunosuppressive therapies, were associated with poor prognosis. Rituximab, when promptly administered, was effective in solving the clinical emergency in most cases unresponsive to steroids and transfusions. Plasma exchange and erythropoietin were valuable options. Above all, in very severe AIHAs a scrupulous and continuous attention by experienced clinicians is required in order to avoid a delay in potentially life-saving strategies.
Keyword(s): Autoimmune hemolytic anemia (AIHA)
Session topic: Publication Only


