BURDEN OF MULTIPLE MYELOMA IN THE UNITED KINGDOM
(Abstract release date: 05/21/15)
EHA Library. Raluy Callado M. 06/12/15; 102777; PB1873
Disclosure(s): EvideraRetrospective Observational Studies

Mireia Raluy Callado
Contributions
Contributions
Abstract
Abstract: PB1873
Type: Publication Only
Background
The introduction of novel agents for the treatment of multiple myeloma (MM) in recent years has been shown to lead in improvements in response and overall survival. However, real world evidence studies on the burden of disease are limited and outdated.
Aims
To describe patient characteristics of newly diagnosed MM patients in the United Kingdom (UK) and to assess disease burden in terms of healthcare resource use.
Methods
Retrospective primary care data from the Clinical Practice Research Datalink (CPRD) linked to the Hospital Episode Statistics (HES) was used. Adult patients with a first diagnosis of MM between Jan 2008-Dec 2012 were identified. Patient characteristics including comorbidities were described at date of diagnosis (index date). Disease-related symptoms, complications and adverse events were described during follow up, as well as primary and secondary care resources, including GP visits and hospitalisations.
Results
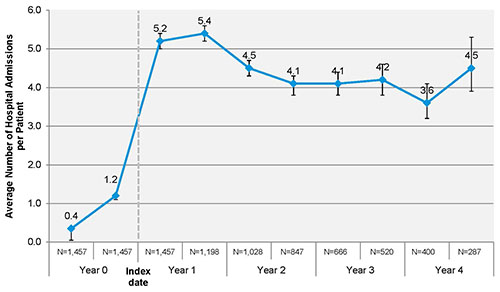
In the CPRD cohort, 1,457 newly diagnosed MM patients were identified and followed up on average for 2.1 years. Of those, 910 (62.5%) were linked to HES (CPRD-HES cohort). Mean age in the CPRD cohort was 71 years (SD: 11.6) and 54.8% were male. Body mass index (BMI) recorded in the 12 months prior diagnosis for 48.5% of the patients was on average 27, classifying them as obese or overweight. The most common comorbidities identified in whole medical history prior diagnosis were renal disease (25.5%), chronic pulmonary disease (19.6%), other malignancies excluding MM (17%) and diabetes without complications (13.1%). During the follow–up period, renal insufficiency was the most common disease symptom (annual incidence: 176.5 per 1,000 patients). Side effects including constipation, vomiting, diarrhoea, syncope, skin rash, and venous thromboembolism were observed at a rate greater than 10 per 100 patients in the first year after diagnosis. GP visits around diagnosis increased from a rate of 4.5 visits/patient (95% Poisson Confidence Intervals [CI]: 4.4-4.6) in 12 to 6 months prior to 8.4 (CI: 8.2-8.5) in the 6 months post diagnosis, and remained high for the entire follow up period (rate: 6.4; CI: 6.4-6.5). Demographic and clinical characteristics of the CPRD-HES cohort were comparable to the overall CPRD cohort; mean age at diagnosis was 71 years (SD: 11.7). A majority (86.6%) of patients in the CPRD-HES cohort incurred at least one hospitalisation post diagnosis (Figure 1). Most hospitalizations were day case admissions (85.6%), with inpatient admissions (14.4%) accounting for the remainder. On average, 4.4 day case admissions per patient per year (SD: 8.8) were encountered in the post-diagnosis period, while the average length of stay for inpatient admissions was 9.8 days (SD=11.85).
Summary
Renal disease and respiratory conditions are common presenting comorbidities among MM patients. The management of disease symptoms, complications and adverse events as well as severe comorbidities leads to increased resource use in both primary and secondary care settings.
Keyword(s): Multiple myeloma
Session topic: Publication Only
Type: Publication Only
Background
The introduction of novel agents for the treatment of multiple myeloma (MM) in recent years has been shown to lead in improvements in response and overall survival. However, real world evidence studies on the burden of disease are limited and outdated.
Aims
To describe patient characteristics of newly diagnosed MM patients in the United Kingdom (UK) and to assess disease burden in terms of healthcare resource use.
Methods
Retrospective primary care data from the Clinical Practice Research Datalink (CPRD) linked to the Hospital Episode Statistics (HES) was used. Adult patients with a first diagnosis of MM between Jan 2008-Dec 2012 were identified. Patient characteristics including comorbidities were described at date of diagnosis (index date). Disease-related symptoms, complications and adverse events were described during follow up, as well as primary and secondary care resources, including GP visits and hospitalisations.
Results
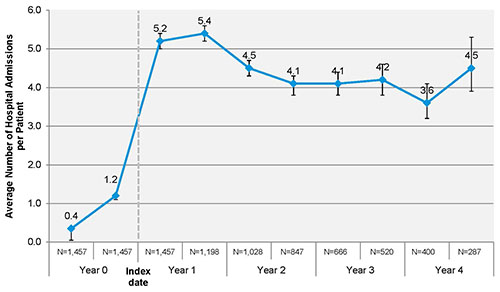
In the CPRD cohort, 1,457 newly diagnosed MM patients were identified and followed up on average for 2.1 years. Of those, 910 (62.5%) were linked to HES (CPRD-HES cohort). Mean age in the CPRD cohort was 71 years (SD: 11.6) and 54.8% were male. Body mass index (BMI) recorded in the 12 months prior diagnosis for 48.5% of the patients was on average 27, classifying them as obese or overweight. The most common comorbidities identified in whole medical history prior diagnosis were renal disease (25.5%), chronic pulmonary disease (19.6%), other malignancies excluding MM (17%) and diabetes without complications (13.1%). During the follow–up period, renal insufficiency was the most common disease symptom (annual incidence: 176.5 per 1,000 patients). Side effects including constipation, vomiting, diarrhoea, syncope, skin rash, and venous thromboembolism were observed at a rate greater than 10 per 100 patients in the first year after diagnosis. GP visits around diagnosis increased from a rate of 4.5 visits/patient (95% Poisson Confidence Intervals [CI]: 4.4-4.6) in 12 to 6 months prior to 8.4 (CI: 8.2-8.5) in the 6 months post diagnosis, and remained high for the entire follow up period (rate: 6.4; CI: 6.4-6.5). Demographic and clinical characteristics of the CPRD-HES cohort were comparable to the overall CPRD cohort; mean age at diagnosis was 71 years (SD: 11.7). A majority (86.6%) of patients in the CPRD-HES cohort incurred at least one hospitalisation post diagnosis (Figure 1). Most hospitalizations were day case admissions (85.6%), with inpatient admissions (14.4%) accounting for the remainder. On average, 4.4 day case admissions per patient per year (SD: 8.8) were encountered in the post-diagnosis period, while the average length of stay for inpatient admissions was 9.8 days (SD=11.85).
Figure 1. Average number of hospital admissions (inpatient and day cases) per patient during 6-month periods prior and post index date (Poisson CI)
Summary
Renal disease and respiratory conditions are common presenting comorbidities among MM patients. The management of disease symptoms, complications and adverse events as well as severe comorbidities leads to increased resource use in both primary and secondary care settings.
Keyword(s): Multiple myeloma
Session topic: Publication Only
Abstract: PB1873
Type: Publication Only
Background
The introduction of novel agents for the treatment of multiple myeloma (MM) in recent years has been shown to lead in improvements in response and overall survival. However, real world evidence studies on the burden of disease are limited and outdated.
Aims
To describe patient characteristics of newly diagnosed MM patients in the United Kingdom (UK) and to assess disease burden in terms of healthcare resource use.
Methods
Retrospective primary care data from the Clinical Practice Research Datalink (CPRD) linked to the Hospital Episode Statistics (HES) was used. Adult patients with a first diagnosis of MM between Jan 2008-Dec 2012 were identified. Patient characteristics including comorbidities were described at date of diagnosis (index date). Disease-related symptoms, complications and adverse events were described during follow up, as well as primary and secondary care resources, including GP visits and hospitalisations.
Results
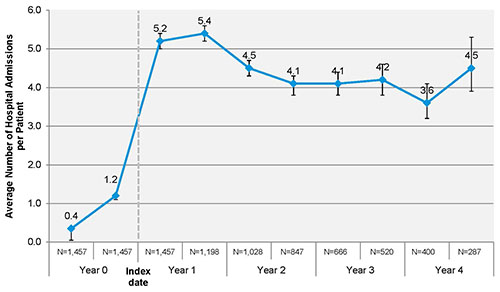
In the CPRD cohort, 1,457 newly diagnosed MM patients were identified and followed up on average for 2.1 years. Of those, 910 (62.5%) were linked to HES (CPRD-HES cohort). Mean age in the CPRD cohort was 71 years (SD: 11.6) and 54.8% were male. Body mass index (BMI) recorded in the 12 months prior diagnosis for 48.5% of the patients was on average 27, classifying them as obese or overweight. The most common comorbidities identified in whole medical history prior diagnosis were renal disease (25.5%), chronic pulmonary disease (19.6%), other malignancies excluding MM (17%) and diabetes without complications (13.1%). During the follow–up period, renal insufficiency was the most common disease symptom (annual incidence: 176.5 per 1,000 patients). Side effects including constipation, vomiting, diarrhoea, syncope, skin rash, and venous thromboembolism were observed at a rate greater than 10 per 100 patients in the first year after diagnosis. GP visits around diagnosis increased from a rate of 4.5 visits/patient (95% Poisson Confidence Intervals [CI]: 4.4-4.6) in 12 to 6 months prior to 8.4 (CI: 8.2-8.5) in the 6 months post diagnosis, and remained high for the entire follow up period (rate: 6.4; CI: 6.4-6.5). Demographic and clinical characteristics of the CPRD-HES cohort were comparable to the overall CPRD cohort; mean age at diagnosis was 71 years (SD: 11.7). A majority (86.6%) of patients in the CPRD-HES cohort incurred at least one hospitalisation post diagnosis (Figure 1). Most hospitalizations were day case admissions (85.6%), with inpatient admissions (14.4%) accounting for the remainder. On average, 4.4 day case admissions per patient per year (SD: 8.8) were encountered in the post-diagnosis period, while the average length of stay for inpatient admissions was 9.8 days (SD=11.85).
Summary
Renal disease and respiratory conditions are common presenting comorbidities among MM patients. The management of disease symptoms, complications and adverse events as well as severe comorbidities leads to increased resource use in both primary and secondary care settings.
Keyword(s): Multiple myeloma
Session topic: Publication Only
Type: Publication Only
Background
The introduction of novel agents for the treatment of multiple myeloma (MM) in recent years has been shown to lead in improvements in response and overall survival. However, real world evidence studies on the burden of disease are limited and outdated.
Aims
To describe patient characteristics of newly diagnosed MM patients in the United Kingdom (UK) and to assess disease burden in terms of healthcare resource use.
Methods
Retrospective primary care data from the Clinical Practice Research Datalink (CPRD) linked to the Hospital Episode Statistics (HES) was used. Adult patients with a first diagnosis of MM between Jan 2008-Dec 2012 were identified. Patient characteristics including comorbidities were described at date of diagnosis (index date). Disease-related symptoms, complications and adverse events were described during follow up, as well as primary and secondary care resources, including GP visits and hospitalisations.
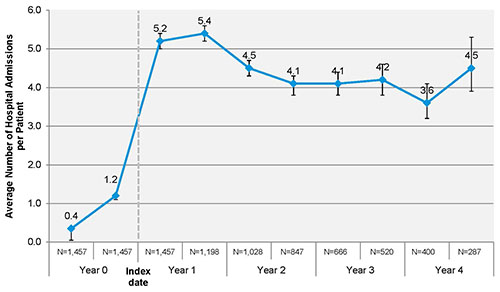
Results
In the CPRD cohort, 1,457 newly diagnosed MM patients were identified and followed up on average for 2.1 years. Of those, 910 (62.5%) were linked to HES (CPRD-HES cohort). Mean age in the CPRD cohort was 71 years (SD: 11.6) and 54.8% were male. Body mass index (BMI) recorded in the 12 months prior diagnosis for 48.5% of the patients was on average 27, classifying them as obese or overweight. The most common comorbidities identified in whole medical history prior diagnosis were renal disease (25.5%), chronic pulmonary disease (19.6%), other malignancies excluding MM (17%) and diabetes without complications (13.1%). During the follow–up period, renal insufficiency was the most common disease symptom (annual incidence: 176.5 per 1,000 patients). Side effects including constipation, vomiting, diarrhoea, syncope, skin rash, and venous thromboembolism were observed at a rate greater than 10 per 100 patients in the first year after diagnosis. GP visits around diagnosis increased from a rate of 4.5 visits/patient (95% Poisson Confidence Intervals [CI]: 4.4-4.6) in 12 to 6 months prior to 8.4 (CI: 8.2-8.5) in the 6 months post diagnosis, and remained high for the entire follow up period (rate: 6.4; CI: 6.4-6.5). Demographic and clinical characteristics of the CPRD-HES cohort were comparable to the overall CPRD cohort; mean age at diagnosis was 71 years (SD: 11.7). A majority (86.6%) of patients in the CPRD-HES cohort incurred at least one hospitalisation post diagnosis (Figure 1). Most hospitalizations were day case admissions (85.6%), with inpatient admissions (14.4%) accounting for the remainder. On average, 4.4 day case admissions per patient per year (SD: 8.8) were encountered in the post-diagnosis period, while the average length of stay for inpatient admissions was 9.8 days (SD=11.85).
Figure 1. Average number of hospital admissions (inpatient and day cases) per patient during 6-month periods prior and post index date (Poisson CI)
Summary
Renal disease and respiratory conditions are common presenting comorbidities among MM patients. The management of disease symptoms, complications and adverse events as well as severe comorbidities leads to increased resource use in both primary and secondary care settings.
Keyword(s): Multiple myeloma
Session topic: Publication Only
{{ help_message }}
{{filter}}


