Hematology laboratory

Contributions
Type: Publication Only
Background
Cytogenetic analysis is an essential step to establish the prognosis in patients with myelodysplastic syndrome (MDS). In our center, the investigation of cytopenia includes a systematic cytogenetic analysis.
Aims
The aim of this work was to compare the efficiency in first intention of bone marrow morphologic analysis to karyotype analysis to reach the diagnosis of myelodysplastic syndrome.
Methods
A monocentric cohort of patients investigated for one or more cytopenia(s) was analysed. Patients diagnosed with MDS with blasts excess, acute leukaemia, bone marrow localization of lymphoma or solid tumor were excluded. Blood, bone marrow smears morphology and karyotype were compared according to the final diagnosis (MDS, immune, metabolic, inflammatory, congenital cytopenia).
Results
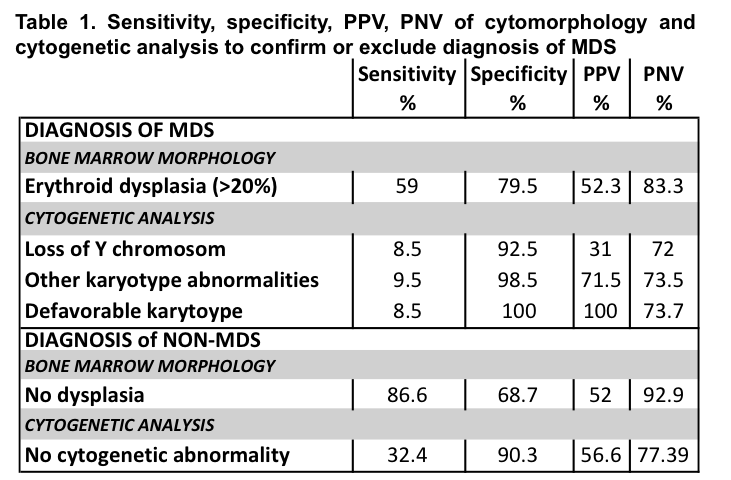
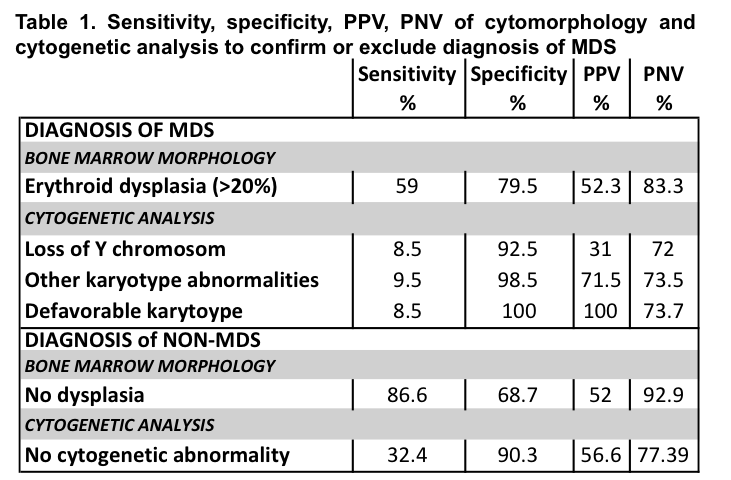
Between 2010 and 2013, samples of 374 patients were analysed. Median age of the whole cohort was 66.8 y.o (1-91). 72% of patients had one cytopenia (mostly anaemia in 50%), 20% were bicytopenic and 8% were pancytopenic. Analysis of bone marrow smears revealed no dysplasia, a uni-or multi-lineage dysplasia or an abnormality of cellularity in respectively 53%, 42% and 5% of cases. Cytogenetic disclosed a normal karyotype in 84% and at least one abnormality in 16% of patients. Loss of Y chromosom, recurring abnormalities and del 5q were the most frequent karyotype abnormalities respectively 7%, 3,7%, 3%. The diagnostic of MDS was retained in 105 patients (29%) whereas 269 patients (71%) were classified as having a differential diagnosis of cytopenia (immune, metabolic, inflammatory, congenital). MDS subtypes were refractory anemia (49%), refractory cytopenias with multilineage dysplasia (20%), refractory cytopenia with unilineage dysplasia (17%), refractory neutropenia (1%), refractory thrombopenia (3%), del 5q syndrome (4%) and MDS-unclassified (6%). In group of MDS patients compared to non-MDS patients, blood test revealed a deeper anaemia (10.2 vs 11 g/dL, p< 0.0001), a higher mean corpuscular volume (94 vs 89 fL, p<0.0001), a higher red-cell distribution width (15.15 vs 13.8, p<0.0001). Then, bone marrow cytomorphology showed more often at least one lineage dysplasia 86.7% vs 30% without dysplasia (p<0.0001) and at least one karyotype abnormality in 32.6% vs 10% without abnormality (p<0.0001). Finally, table 1 summarizes sensitivity, specificity, positive predictive (PPV) and negative value (PNV) of morphological and cytogenetic analyses for the diagnosis of MDS
Summary
For the diagnosis of myelodysplastic syndrome, cytomorphology of bone marrow is more sensitive but less specific than cytogenetics. Our results suggest that in case of cytopenia without blast excess or malignant infiltration, blood and bone marrow smears microscopic examination could be performed frontline and cytogenetic examination could be delayed at the time of morphology confirmation after 1 to 3 months.
Keyword(s): Bone marrow biopsy, Cytogenetics, Myelodysplasia
Type: Publication Only
Background
Cytogenetic analysis is an essential step to establish the prognosis in patients with myelodysplastic syndrome (MDS). In our center, the investigation of cytopenia includes a systematic cytogenetic analysis.
Aims
The aim of this work was to compare the efficiency in first intention of bone marrow morphologic analysis to karyotype analysis to reach the diagnosis of myelodysplastic syndrome.
Methods
A monocentric cohort of patients investigated for one or more cytopenia(s) was analysed. Patients diagnosed with MDS with blasts excess, acute leukaemia, bone marrow localization of lymphoma or solid tumor were excluded. Blood, bone marrow smears morphology and karyotype were compared according to the final diagnosis (MDS, immune, metabolic, inflammatory, congenital cytopenia).
Results
Between 2010 and 2013, samples of 374 patients were analysed. Median age of the whole cohort was 66.8 y.o (1-91). 72% of patients had one cytopenia (mostly anaemia in 50%), 20% were bicytopenic and 8% were pancytopenic. Analysis of bone marrow smears revealed no dysplasia, a uni-or multi-lineage dysplasia or an abnormality of cellularity in respectively 53%, 42% and 5% of cases. Cytogenetic disclosed a normal karyotype in 84% and at least one abnormality in 16% of patients. Loss of Y chromosom, recurring abnormalities and del 5q were the most frequent karyotype abnormalities respectively 7%, 3,7%, 3%. The diagnostic of MDS was retained in 105 patients (29%) whereas 269 patients (71%) were classified as having a differential diagnosis of cytopenia (immune, metabolic, inflammatory, congenital). MDS subtypes were refractory anemia (49%), refractory cytopenias with multilineage dysplasia (20%), refractory cytopenia with unilineage dysplasia (17%), refractory neutropenia (1%), refractory thrombopenia (3%), del 5q syndrome (4%) and MDS-unclassified (6%). In group of MDS patients compared to non-MDS patients, blood test revealed a deeper anaemia (10.2 vs 11 g/dL, p< 0.0001), a higher mean corpuscular volume (94 vs 89 fL, p<0.0001), a higher red-cell distribution width (15.15 vs 13.8, p<0.0001). Then, bone marrow cytomorphology showed more often at least one lineage dysplasia 86.7% vs 30% without dysplasia (p<0.0001) and at least one karyotype abnormality in 32.6% vs 10% without abnormality (p<0.0001). Finally, table 1 summarizes sensitivity, specificity, positive predictive (PPV) and negative value (PNV) of morphological and cytogenetic analyses for the diagnosis of MDS
Summary
For the diagnosis of myelodysplastic syndrome, cytomorphology of bone marrow is more sensitive but less specific than cytogenetics. Our results suggest that in case of cytopenia without blast excess or malignant infiltration, blood and bone marrow smears microscopic examination could be performed frontline and cytogenetic examination could be delayed at the time of morphology confirmation after 1 to 3 months.
Keyword(s): Bone marrow biopsy, Cytogenetics, Myelodysplasia