Pediatric Hematology

Contributions
Type: Publication Only
Background
Gastrointestinal complications are common following hematopoietic stem cell transplantation (HSCT); however angiodysplasia is not well characterized in terms of its association with HSCT and only a few reports of angiodysplasia in transplant recipients are available, all of them are adults.
Aims
Here we report a 7 years old child with a massive lower gastrointestinal bleeding, caused by angiodysplasia (vascular ectasia) following HSCT. To our knowledge, this is the first reported pediatric case demonstrating the association of angiodysplasia with HSCT and successfully controlled by angioembolization.
Methods
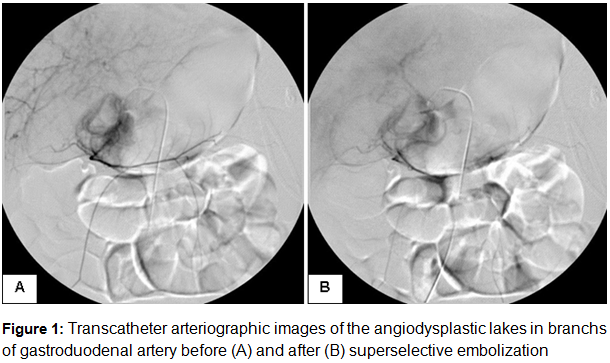
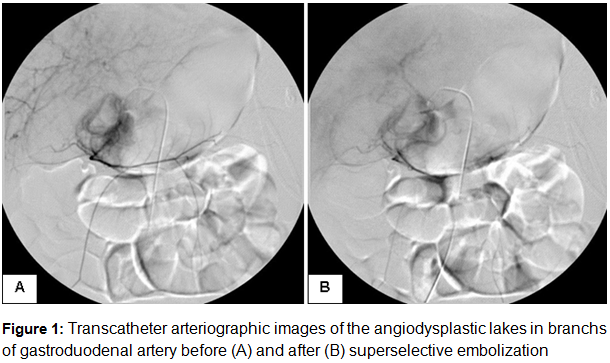
The patient was a 6-year-old boy who underwent HSCT for relapsed acute lymphoblastic leukemia. He was in remission at the time of transplant. Preparative regimen consisted of 12 Gy total body irradiation and 60 mg/kg etoposide. He received 2,4x106/kg CD34+ stem cells from his well-matched father (one antigen mismatched at HLA-C). Cyclosporin was administered for GVHD prophylaxis. Full engraftment was achieved with neutrophil, platelet and erythrocyte recovery being 13, 20 and 27 days respectively. On the 14th day of transplantation grade IV acute graft-versus-host disease (GVHD) was developed (skin stage III, liver and gastrointestinal tract stage IV). Skin manifestations were resolved, but liver and gastrointestinal GVHD went on depite prednisolone therapy and the increase of cyclosporin. However, thrombotic microangiopathy (TMA) was developed on the 19th day and resolution was not achieved despite the switch of cyclosporin to mycophenolate mofetil. He underwent therapeutic plasma exchange sessions on alternate days. The resolution was achieved after 14 sessions, liver GVHD was also resolved, but gastrointestinal symptoms went on with recurrent massive gastrointestinal bleeding despite therapies including octreotide, recombinant human coagulation Factor VIIa and third party mesenchymal stem cells. The localization of the gastrointestinal bleeding couldn’t be identified despite nuclear medicine scan, endoscopy and colonoscopy. The localization of the bleeding couldn’t be identified with transcatheter arteriography also, but there were seen angiodysplastic lakes in branchs of celiac, gastroduodenal and superior mesenteric artery (Figure1). With the suspicion of these lakes may be the origin of bleedings, superselective embolization was performed and gastrointestinal bleeding episodes were resolved completely without any complication. Occult gastrointestinal bleeing was also became negative after ten days of the embolization and he was discharged on the 130th day of HSCT.
Results
In the literature on the subject, it is observed that HSCT associated gastric vascular ectasias are with a prior TMA episode and suggested that local endothelial injury and subsequent local thrombosis in TMA may obstruct submucosal blood vessels and eventually lead to development of vascular ectasia. The fibrin thrombi and/or ectasia in mucosal vessels observed histologically in these patients supported their hypothesis
Summary
In conclusion, angiodysplasia is a rare but important cause of recurrent intestinal bleeding in children and should be kept in mind as a diagnostic possibility especially in HSCT patients who have a history of TMA. Early diagnosis of this rare lesion is important to avoid a possible fatal outcome and thus the physician should be aware of this lesion as a rare cause of intestinal bleeding in children.
Keyword(s): Bleeding, Gastrointestinal GVHD, Thrombotic microangiopathy, Transplant-related mortality
Type: Publication Only
Background
Gastrointestinal complications are common following hematopoietic stem cell transplantation (HSCT); however angiodysplasia is not well characterized in terms of its association with HSCT and only a few reports of angiodysplasia in transplant recipients are available, all of them are adults.
Aims
Here we report a 7 years old child with a massive lower gastrointestinal bleeding, caused by angiodysplasia (vascular ectasia) following HSCT. To our knowledge, this is the first reported pediatric case demonstrating the association of angiodysplasia with HSCT and successfully controlled by angioembolization.
Methods
The patient was a 6-year-old boy who underwent HSCT for relapsed acute lymphoblastic leukemia. He was in remission at the time of transplant. Preparative regimen consisted of 12 Gy total body irradiation and 60 mg/kg etoposide. He received 2,4x106/kg CD34+ stem cells from his well-matched father (one antigen mismatched at HLA-C). Cyclosporin was administered for GVHD prophylaxis. Full engraftment was achieved with neutrophil, platelet and erythrocyte recovery being 13, 20 and 27 days respectively. On the 14th day of transplantation grade IV acute graft-versus-host disease (GVHD) was developed (skin stage III, liver and gastrointestinal tract stage IV). Skin manifestations were resolved, but liver and gastrointestinal GVHD went on depite prednisolone therapy and the increase of cyclosporin. However, thrombotic microangiopathy (TMA) was developed on the 19th day and resolution was not achieved despite the switch of cyclosporin to mycophenolate mofetil. He underwent therapeutic plasma exchange sessions on alternate days. The resolution was achieved after 14 sessions, liver GVHD was also resolved, but gastrointestinal symptoms went on with recurrent massive gastrointestinal bleeding despite therapies including octreotide, recombinant human coagulation Factor VIIa and third party mesenchymal stem cells. The localization of the gastrointestinal bleeding couldn’t be identified despite nuclear medicine scan, endoscopy and colonoscopy. The localization of the bleeding couldn’t be identified with transcatheter arteriography also, but there were seen angiodysplastic lakes in branchs of celiac, gastroduodenal and superior mesenteric artery (Figure1). With the suspicion of these lakes may be the origin of bleedings, superselective embolization was performed and gastrointestinal bleeding episodes were resolved completely without any complication. Occult gastrointestinal bleeing was also became negative after ten days of the embolization and he was discharged on the 130th day of HSCT.
Results
In the literature on the subject, it is observed that HSCT associated gastric vascular ectasias are with a prior TMA episode and suggested that local endothelial injury and subsequent local thrombosis in TMA may obstruct submucosal blood vessels and eventually lead to development of vascular ectasia. The fibrin thrombi and/or ectasia in mucosal vessels observed histologically in these patients supported their hypothesis
Summary
In conclusion, angiodysplasia is a rare but important cause of recurrent intestinal bleeding in children and should be kept in mind as a diagnostic possibility especially in HSCT patients who have a history of TMA. Early diagnosis of this rare lesion is important to avoid a possible fatal outcome and thus the physician should be aware of this lesion as a rare cause of intestinal bleeding in children.
Keyword(s): Bleeding, Gastrointestinal GVHD, Thrombotic microangiopathy, Transplant-related mortality