Contributions
Type: Publication Only
Background
The mutation of the myeloid differentiation primary response gene 88 (MYD88) at amino acid position 265 leading to a change from leucine to proline (L256P) is present in approximately one-third of patients (pts) with activated B-cell–like types of diffuse large B-cell lymphoma (ABC-DLBCL) and rarely occurs in pts with other subtypes of DLBCL. Considering the published data, patients with MYD88 DLBCL treated by standard chemotherapy (CHOP and CHOP-like regimens), was associated with an unfavorable outcome.
Aims
To identify the clinical and prognostic value of the MYD88 L256P mutation in pts with ABC-DLBCL who received treatment in the National Research Center for Hematology during 2008-2014.
Methods
Thirty-two newly diagnosed pts with ABC-DLBCL were selected for the study. The diagnosis of ABC-DLBCL was established according to the World Health Organization 2008 classification. DNA from 28 cryopreserved and 4 formalin-fixed paraffin-embedded tumor samples were available for our study. The screening for MYD88 L256P mutation was performed by Sanger sequencing and allele-specific PCR.
Results
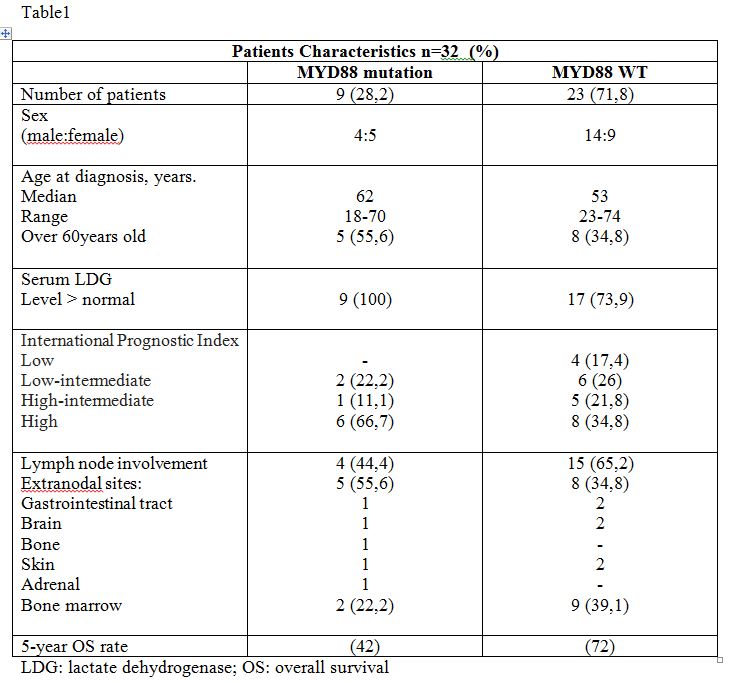
Thirty-two pts with ABC-DLBCL (median age 54,5 years (range 18-74), 18 males and 14 females) were tested for MYD88 mutation. MYD88 L265P mutation was found in 28,2% (9/32) of pts. There was just a slight predominance of the female sex for MYD88 L265P positive group (5:4) as compared to MYD88 negative group (9:14). According to the Ann Arbor classification, approximately 55% pts had stage IV of the disease in both groups. Sixty-six percent of the pts with MYD88 mutated DLBCL were classified as the high risk group by the international prognostic index (IPI) vs 8 (34,8%) pts MYD88 unmutated DLBCL. In addition, 17 of 23 pts (73,9%) with MYD88 wild type DLBCL had elevated lactate dehydrogenase (LDH) levels versus 100% of pts with MYD88-positive DLBCL. Among MYD88 positive group 5/9 (55,6%) pts had extranodal lesions: central nervous system, skin, gastrointestinal tract, adrenal gland, bone and soft tissue, as compared to cases without MYD88 DLBCL 8/23 (34,8%). The clinical characterictics of the pts are summarized in Table 1. All pts received high-dose chemotherapy, 6/9 MYD88 mutated pts achieve complete remission after initial treatment, one of them experienced disease relapse with nasopharynx, bone marrow, vertebral involvement 45 months after the diagnosis, median follow-up was 41 (range 11-83) months. Three pts had died of progressing lymphoma. Out of 23 pts with MYD88 wild type DLBCL, 17 pts achieved complete remission (median follow-up 54 months, range 11-90), 2 pts had early relapse and 4 pts were refractory. Overall survival (OS) was better in pts with MYD88 unmutated DLBCL than pts with MYD88 positive DLBCL (5-year OS, 72% vs 42%).
Summary
Our study has demonstrated that the presence of MYD88 L256P mutation in pts with ABC-DLBCL is associated with worse OS probability. An analysis of treatment outcomes revealed no statistically significant differences in OS because of the small number of pts enrolled in study. MYD88 L265P DLBCL presented with higher number of extranodal involvement, IPI high risk and older age as compared to MYD88 wild type DLBCL. We plan to increase patient recruitment in our research, continue to analysis MYD88 mutation in ABC DLBCL and try to improve treatment strategy in patients with poor-prognosis DLBCL.
Keyword(s): Diffuse large B cell lymphoma, High-dose therapy, Mutation
Type: Publication Only
Background
The mutation of the myeloid differentiation primary response gene 88 (MYD88) at amino acid position 265 leading to a change from leucine to proline (L256P) is present in approximately one-third of patients (pts) with activated B-cell–like types of diffuse large B-cell lymphoma (ABC-DLBCL) and rarely occurs in pts with other subtypes of DLBCL. Considering the published data, patients with MYD88 DLBCL treated by standard chemotherapy (CHOP and CHOP-like regimens), was associated with an unfavorable outcome.
Aims
To identify the clinical and prognostic value of the MYD88 L256P mutation in pts with ABC-DLBCL who received treatment in the National Research Center for Hematology during 2008-2014.
Methods
Thirty-two newly diagnosed pts with ABC-DLBCL were selected for the study. The diagnosis of ABC-DLBCL was established according to the World Health Organization 2008 classification. DNA from 28 cryopreserved and 4 formalin-fixed paraffin-embedded tumor samples were available for our study. The screening for MYD88 L256P mutation was performed by Sanger sequencing and allele-specific PCR.
Results
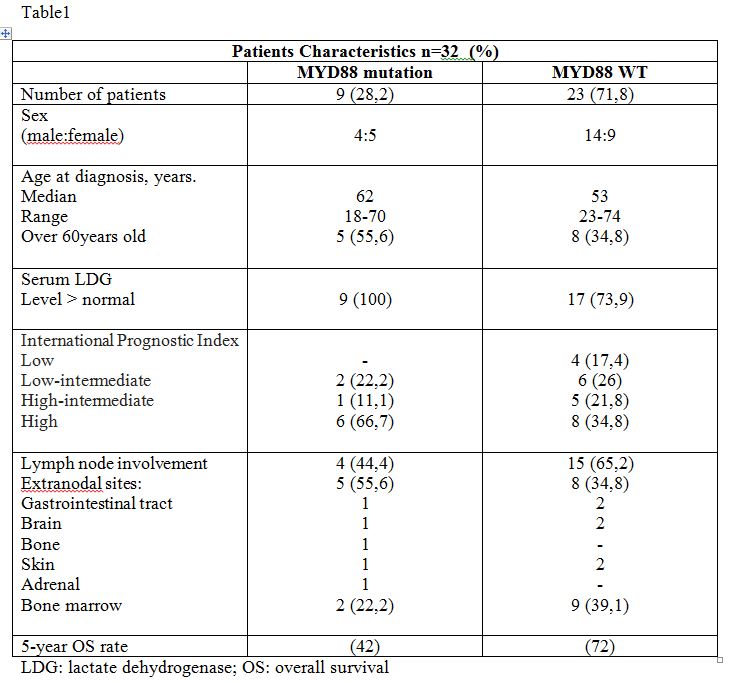
Thirty-two pts with ABC-DLBCL (median age 54,5 years (range 18-74), 18 males and 14 females) were tested for MYD88 mutation. MYD88 L265P mutation was found in 28,2% (9/32) of pts. There was just a slight predominance of the female sex for MYD88 L265P positive group (5:4) as compared to MYD88 negative group (9:14). According to the Ann Arbor classification, approximately 55% pts had stage IV of the disease in both groups. Sixty-six percent of the pts with MYD88 mutated DLBCL were classified as the high risk group by the international prognostic index (IPI) vs 8 (34,8%) pts MYD88 unmutated DLBCL. In addition, 17 of 23 pts (73,9%) with MYD88 wild type DLBCL had elevated lactate dehydrogenase (LDH) levels versus 100% of pts with MYD88-positive DLBCL. Among MYD88 positive group 5/9 (55,6%) pts had extranodal lesions: central nervous system, skin, gastrointestinal tract, adrenal gland, bone and soft tissue, as compared to cases without MYD88 DLBCL 8/23 (34,8%). The clinical characterictics of the pts are summarized in Table 1. All pts received high-dose chemotherapy, 6/9 MYD88 mutated pts achieve complete remission after initial treatment, one of them experienced disease relapse with nasopharynx, bone marrow, vertebral involvement 45 months after the diagnosis, median follow-up was 41 (range 11-83) months. Three pts had died of progressing lymphoma. Out of 23 pts with MYD88 wild type DLBCL, 17 pts achieved complete remission (median follow-up 54 months, range 11-90), 2 pts had early relapse and 4 pts were refractory. Overall survival (OS) was better in pts with MYD88 unmutated DLBCL than pts with MYD88 positive DLBCL (5-year OS, 72% vs 42%).
Summary
Our study has demonstrated that the presence of MYD88 L256P mutation in pts with ABC-DLBCL is associated with worse OS probability. An analysis of treatment outcomes revealed no statistically significant differences in OS because of the small number of pts enrolled in study. MYD88 L265P DLBCL presented with higher number of extranodal involvement, IPI high risk and older age as compared to MYD88 wild type DLBCL. We plan to increase patient recruitment in our research, continue to analysis MYD88 mutation in ABC DLBCL and try to improve treatment strategy in patients with poor-prognosis DLBCL.
Keyword(s): Diffuse large B cell lymphoma, High-dose therapy, Mutation