LOW HEMOGLOBIN LEVELS AT DIAGNOSIS ARE ASSOCIATED WITH WORSE TREATMENT RESPONSES AND EVENT FREE SURVIVAL IN CHRONIC MYELOID LEUKEMIA PATIENTS IN CHRONIC PHASE RECEIVING TYROSINE KINASE INHIBITORS
(Abstract release date: 05/21/15)
EHA Library. Ko P. 06/12/15; 102600; PB1754
Disclosure(s): Taipei Veteran General HospitalDivision of Hematology and Oncology

Mr. Po-Shen Ko
Contributions
Contributions
Abstract
Abstract: PB1754
Type: Publication Only
Background
SPECIAL;Despite progress in prognosis of patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitors (TKI), values of current available three prognostic scoring systems, namely Sokal, Hasford and EUTOS scores, for predicting survival outcomes and treatment response remained inconclusive. Current Sokal and Hasford score developed in pre-TKI era and they both included many baseline clinical variables but without baseline hemoglobin levels, a seldomly discussed variable. The value of baseline hemoglobin levels for predicting treatment responses and survival outcomes might be worthy to be reevaluated.
Aims
This study aims to exam the role of hemoglobin level at diagnosis in association with survival outcomes and treatment responses in chronic myeloid leukemia patients in chronic phase (CML-CP) receiving frontline TKIs and to validate the three scoring systems.
Methods
SPECIAL;A total 172 consecutive patients with CML-CP patients were screened retrospectively from January 2001 to April 2014. Patients who previously recieved interferon-alpha or any chemotherapeutic agents or in combination with TKIs treatment, patients who were lost follow-up within 3 months of diagnosis, and patisnts who had no adequate data to calculate baseline risk socres were excluded. 143 patients were enrolled to further analysis after screening. The cut-offs of baseline hemoglobin level were defined as 12.3 mg/dl for male and 9.0 mg/dl for female sperately in consideration for gender difference in hemoglobin levels by adopting the receiver oprator characteristic (ROC) curve method.
Results
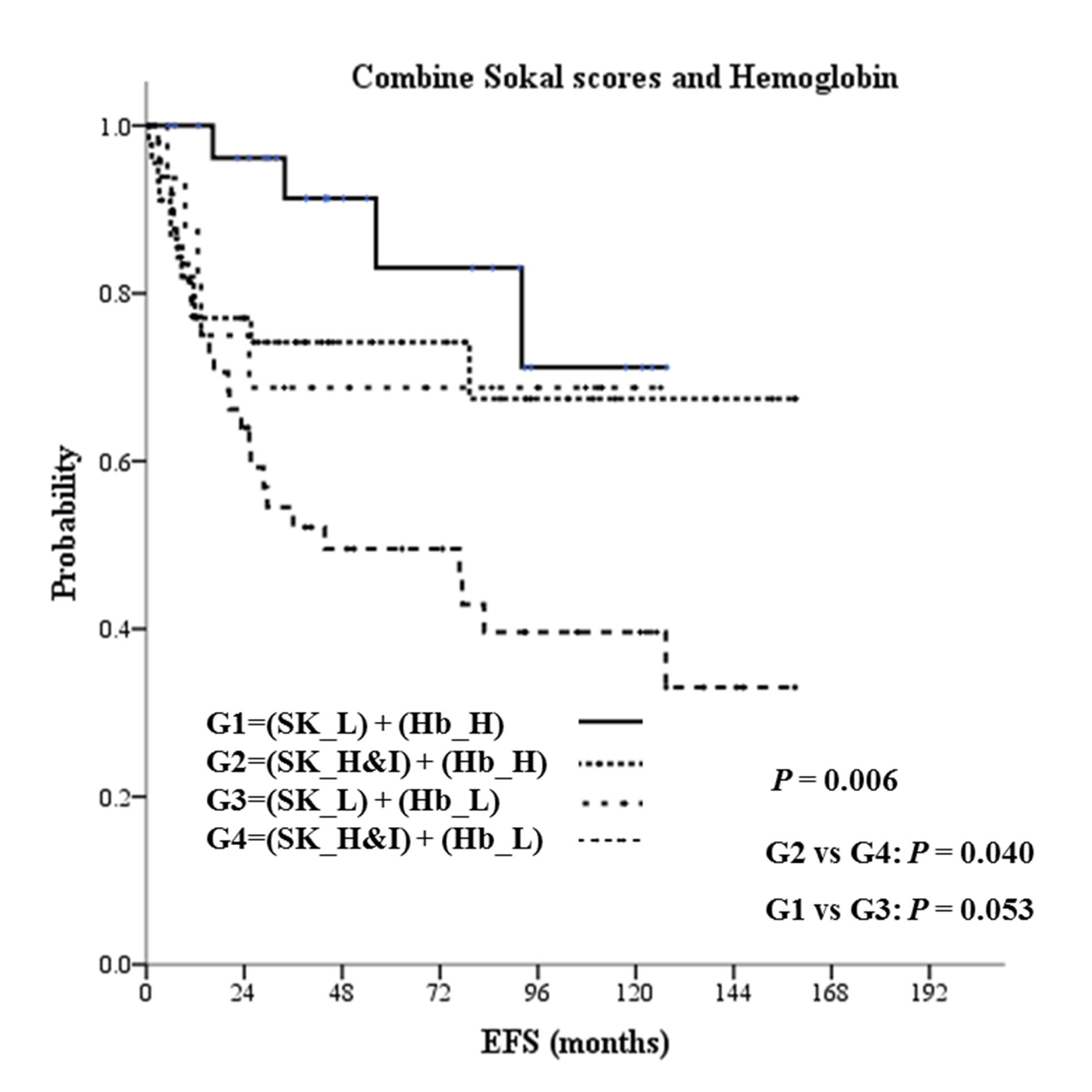
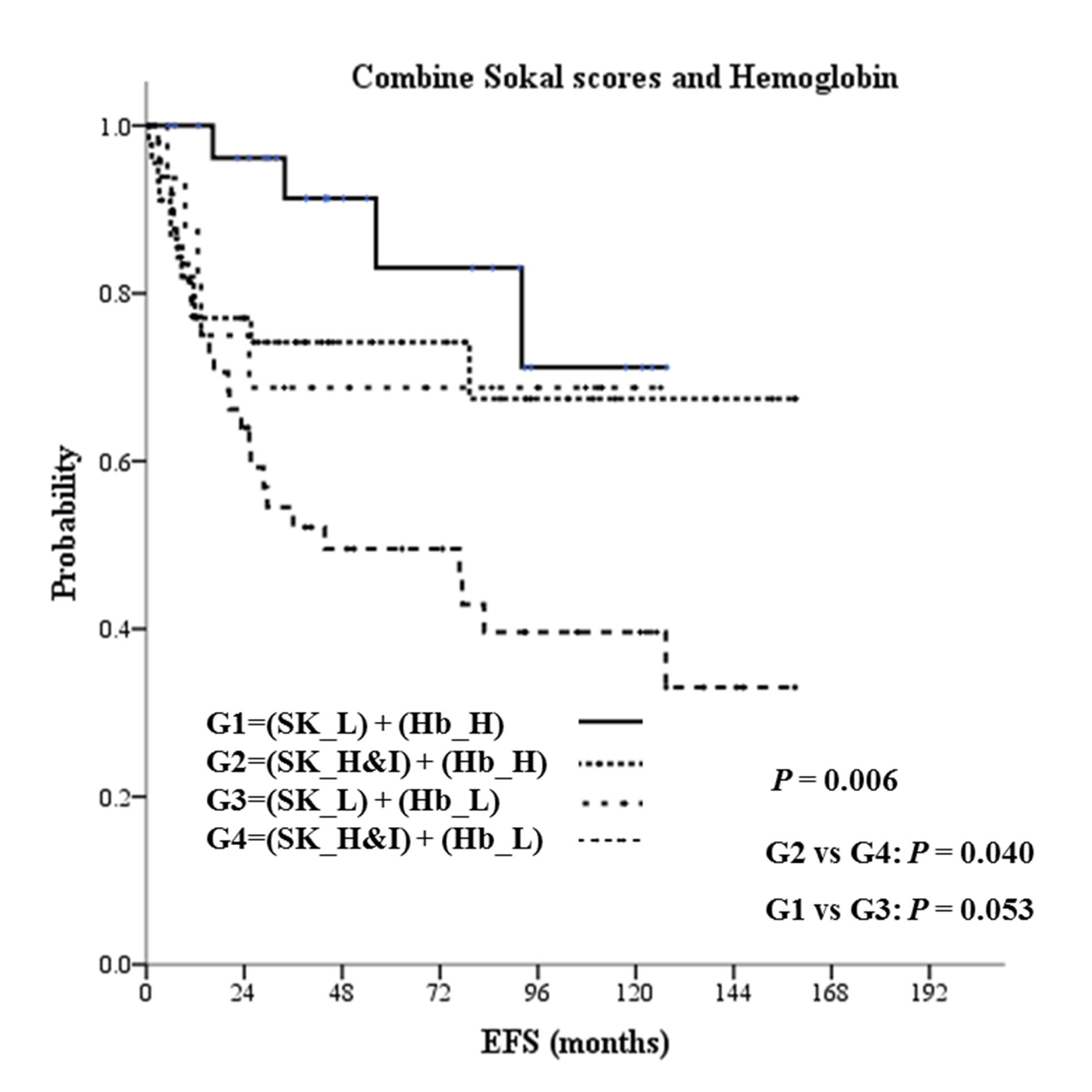
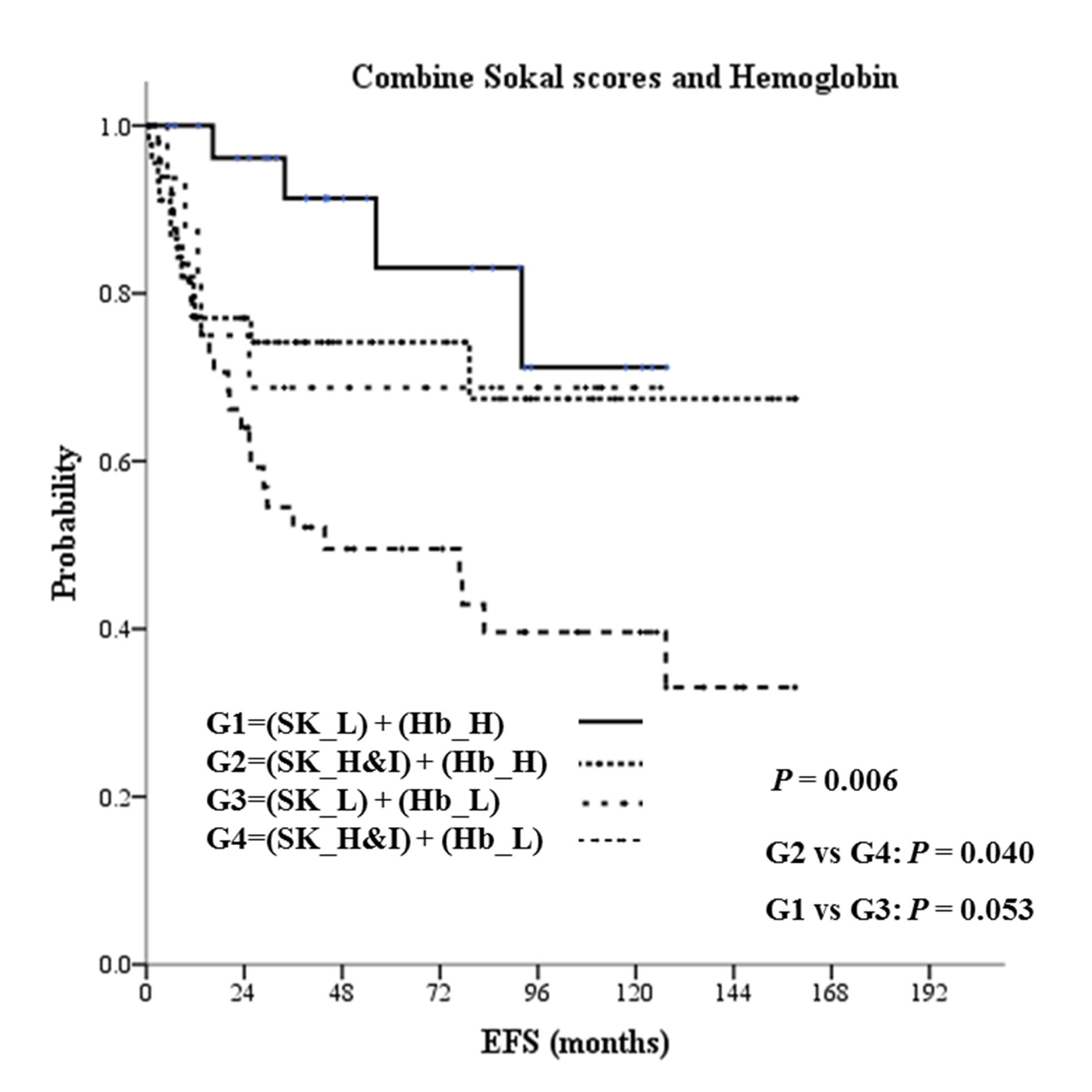
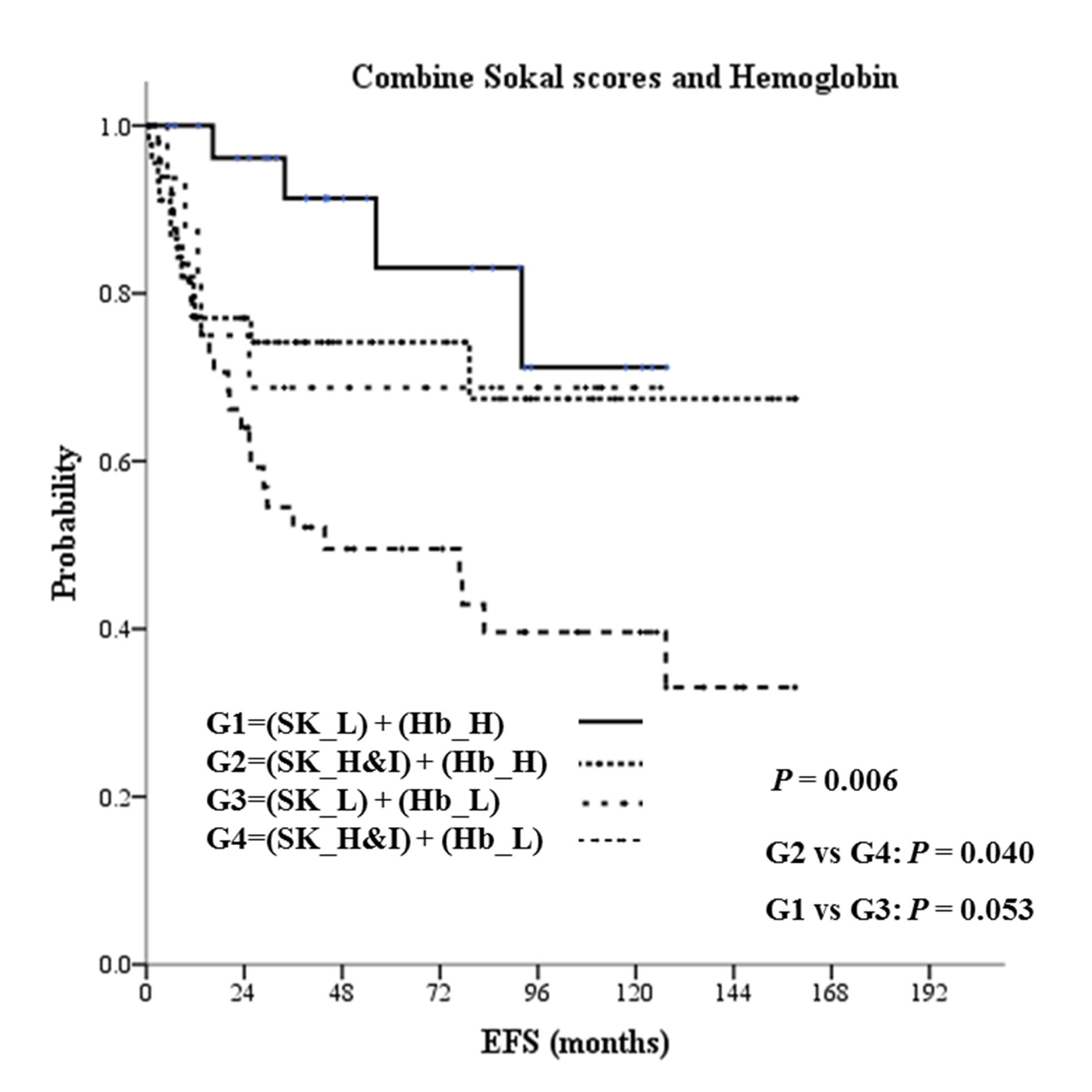
With a median follow-up of 54.0 months, 5-year overall survival (OS), progression-free survival (PFS), and event-free survival (EFS) were 87.5%, 85.9% and 66.8%. We found Sokal and Hasford, but not EUTOS score were predictive for difference in EFS and PFS; however, none of the three scoring systems were predictive for difference in OS. Lower baseline hemoglobin levels was an independent adverse factors for EFS (hazard ration 2.06; 95% confidence interval 1.12-3.78, p=0.019) and associated with worse treatment responses: the proportion of patients with lower versus higher hemoglobin levels achieving optimal responses were 52.2 % vs 71.1 % for 3-month early molecular response (p=0.021), 20.0% vs 51.4% for 6-month complete cytogenetic respone (p<0.001), and 18.0% vs 45.1% for 12-month major molecular response (p<0.001). Furthermore, combining hemogobin level and Sokal score further distinguised a population at risk for worse EFS and treatment responses.
Summary
The results highlights the need for revisiting tradition CML scoring systems in the TKI era and suggests baseline hemoglobin levels at diagnosis might be considered for new scoring systems.
Keyword(s): Chronic myeloid leukemia, Hemoglobin, Prognostic factor, Survival prediction
Type: Publication Only
Background
SPECIAL;Despite progress in prognosis of patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitors (TKI), values of current available three prognostic scoring systems, namely Sokal, Hasford and EUTOS scores, for predicting survival outcomes and treatment response remained inconclusive. Current Sokal and Hasford score developed in pre-TKI era and they both included many baseline clinical variables but without baseline hemoglobin levels, a seldomly discussed variable. The value of baseline hemoglobin levels for predicting treatment responses and survival outcomes might be worthy to be reevaluated.
Aims
This study aims to exam the role of hemoglobin level at diagnosis in association with survival outcomes and treatment responses in chronic myeloid leukemia patients in chronic phase (CML-CP) receiving frontline TKIs and to validate the three scoring systems.
Methods
SPECIAL;A total 172 consecutive patients with CML-CP patients were screened retrospectively from January 2001 to April 2014. Patients who previously recieved interferon-alpha or any chemotherapeutic agents or in combination with TKIs treatment, patients who were lost follow-up within 3 months of diagnosis, and patisnts who had no adequate data to calculate baseline risk socres were excluded. 143 patients were enrolled to further analysis after screening. The cut-offs of baseline hemoglobin level were defined as 12.3 mg/dl for male and 9.0 mg/dl for female sperately in consideration for gender difference in hemoglobin levels by adopting the receiver oprator characteristic (ROC) curve method.
Results
With a median follow-up of 54.0 months, 5-year overall survival (OS), progression-free survival (PFS), and event-free survival (EFS) were 87.5%, 85.9% and 66.8%. We found Sokal and Hasford, but not EUTOS score were predictive for difference in EFS and PFS; however, none of the three scoring systems were predictive for difference in OS. Lower baseline hemoglobin levels was an independent adverse factors for EFS (hazard ration 2.06; 95% confidence interval 1.12-3.78, p=0.019) and associated with worse treatment responses: the proportion of patients with lower versus higher hemoglobin levels achieving optimal responses were 52.2 % vs 71.1 % for 3-month early molecular response (p=0.021), 20.0% vs 51.4% for 6-month complete cytogenetic respone (p<0.001), and 18.0% vs 45.1% for 12-month major molecular response (p<0.001). Furthermore, combining hemogobin level and Sokal score further distinguised a population at risk for worse EFS and treatment responses.
Summary
The results highlights the need for revisiting tradition CML scoring systems in the TKI era and suggests baseline hemoglobin levels at diagnosis might be considered for new scoring systems.
Keyword(s): Chronic myeloid leukemia, Hemoglobin, Prognostic factor, Survival prediction
Abstract: PB1754
Type: Publication Only
Background
SPECIAL;Despite progress in prognosis of patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitors (TKI), values of current available three prognostic scoring systems, namely Sokal, Hasford and EUTOS scores, for predicting survival outcomes and treatment response remained inconclusive. Current Sokal and Hasford score developed in pre-TKI era and they both included many baseline clinical variables but without baseline hemoglobin levels, a seldomly discussed variable. The value of baseline hemoglobin levels for predicting treatment responses and survival outcomes might be worthy to be reevaluated.
Aims
This study aims to exam the role of hemoglobin level at diagnosis in association with survival outcomes and treatment responses in chronic myeloid leukemia patients in chronic phase (CML-CP) receiving frontline TKIs and to validate the three scoring systems.
Methods
SPECIAL;A total 172 consecutive patients with CML-CP patients were screened retrospectively from January 2001 to April 2014. Patients who previously recieved interferon-alpha or any chemotherapeutic agents or in combination with TKIs treatment, patients who were lost follow-up within 3 months of diagnosis, and patisnts who had no adequate data to calculate baseline risk socres were excluded. 143 patients were enrolled to further analysis after screening. The cut-offs of baseline hemoglobin level were defined as 12.3 mg/dl for male and 9.0 mg/dl for female sperately in consideration for gender difference in hemoglobin levels by adopting the receiver oprator characteristic (ROC) curve method.
Results
With a median follow-up of 54.0 months, 5-year overall survival (OS), progression-free survival (PFS), and event-free survival (EFS) were 87.5%, 85.9% and 66.8%. We found Sokal and Hasford, but not EUTOS score were predictive for difference in EFS and PFS; however, none of the three scoring systems were predictive for difference in OS. Lower baseline hemoglobin levels was an independent adverse factors for EFS (hazard ration 2.06; 95% confidence interval 1.12-3.78, p=0.019) and associated with worse treatment responses: the proportion of patients with lower versus higher hemoglobin levels achieving optimal responses were 52.2 % vs 71.1 % for 3-month early molecular response (p=0.021), 20.0% vs 51.4% for 6-month complete cytogenetic respone (p<0.001), and 18.0% vs 45.1% for 12-month major molecular response (p<0.001). Furthermore, combining hemogobin level and Sokal score further distinguised a population at risk for worse EFS and treatment responses.
Summary
The results highlights the need for revisiting tradition CML scoring systems in the TKI era and suggests baseline hemoglobin levels at diagnosis might be considered for new scoring systems.
Keyword(s): Chronic myeloid leukemia, Hemoglobin, Prognostic factor, Survival prediction
Type: Publication Only
Background
SPECIAL;Despite progress in prognosis of patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitors (TKI), values of current available three prognostic scoring systems, namely Sokal, Hasford and EUTOS scores, for predicting survival outcomes and treatment response remained inconclusive. Current Sokal and Hasford score developed in pre-TKI era and they both included many baseline clinical variables but without baseline hemoglobin levels, a seldomly discussed variable. The value of baseline hemoglobin levels for predicting treatment responses and survival outcomes might be worthy to be reevaluated.
Aims
This study aims to exam the role of hemoglobin level at diagnosis in association with survival outcomes and treatment responses in chronic myeloid leukemia patients in chronic phase (CML-CP) receiving frontline TKIs and to validate the three scoring systems.
Methods
SPECIAL;A total 172 consecutive patients with CML-CP patients were screened retrospectively from January 2001 to April 2014. Patients who previously recieved interferon-alpha or any chemotherapeutic agents or in combination with TKIs treatment, patients who were lost follow-up within 3 months of diagnosis, and patisnts who had no adequate data to calculate baseline risk socres were excluded. 143 patients were enrolled to further analysis after screening. The cut-offs of baseline hemoglobin level were defined as 12.3 mg/dl for male and 9.0 mg/dl for female sperately in consideration for gender difference in hemoglobin levels by adopting the receiver oprator characteristic (ROC) curve method.
Results
With a median follow-up of 54.0 months, 5-year overall survival (OS), progression-free survival (PFS), and event-free survival (EFS) were 87.5%, 85.9% and 66.8%. We found Sokal and Hasford, but not EUTOS score were predictive for difference in EFS and PFS; however, none of the three scoring systems were predictive for difference in OS. Lower baseline hemoglobin levels was an independent adverse factors for EFS (hazard ration 2.06; 95% confidence interval 1.12-3.78, p=0.019) and associated with worse treatment responses: the proportion of patients with lower versus higher hemoglobin levels achieving optimal responses were 52.2 % vs 71.1 % for 3-month early molecular response (p=0.021), 20.0% vs 51.4% for 6-month complete cytogenetic respone (p<0.001), and 18.0% vs 45.1% for 12-month major molecular response (p<0.001). Furthermore, combining hemogobin level and Sokal score further distinguised a population at risk for worse EFS and treatment responses.
Summary
The results highlights the need for revisiting tradition CML scoring systems in the TKI era and suggests baseline hemoglobin levels at diagnosis might be considered for new scoring systems.
Keyword(s): Chronic myeloid leukemia, Hemoglobin, Prognostic factor, Survival prediction
{{ help_message }}
{{filter}}


