
Contributions
Abstract: EP1222
Type: E-Poster Presentation
Session title: Sickle cell disease
Background
Sickle cell disease (SCD) is a global health burden that has been largely neglected. Despite improvements in diagnosis, treatment and management over the past few decades, SCD morbidity including vaso-occlusive crises (VOCs) remains high. VOCs, the hallmark of SCD, are the primary cause of hospitalization for SCD patients, and are associated with significant morbidity and mortality. Evidence regarding potential risk factors for hospitalization due to VOC (H-VOC) including commonly measured blood markers is limited.
Aims
To assess whether selected factors are associated with the rate of H-VOC and hospital length of stay by performing a retrospective analysis of data collected prospectively during a 3-year, multicenter, observational US study (NCT01220115) that aimed to better understand disease burden and management of SCD in patients aged ≥2 years.
Methods
Out of a total of 498 recruited patients, 202 aged ≥16 years and for whom patient-reported hospital admission data were available were included in this analysis. Negative binomial regression (adjusted for age, sex, and SCD genotype) was used to examine the association of selected baseline characteristics (ie body mass index, hemoglobin, ferritin, transaminases, and any history [received in the preceding 12 months] of opioids, hydroxyurea, transfusion, and H-VOC) with the frequency and length of stay of H-VOC in SCD patients.
Results
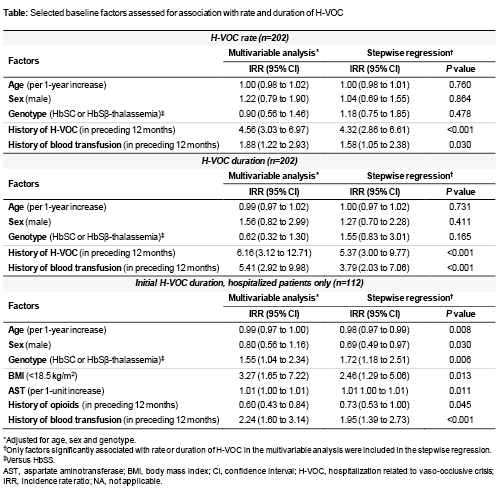
Overall, 71% of patients had a HbSS genotype, 98% were Black or African American and 51% were female. The median age of the cohort was 31 years (interquartile range [IQR] 22–41). At baseline, 36% of patients had received opioids, 14% had received hydroxyurea and 51% had received transfusions in the previous 12 months, comprising 30% who had received 1–5 transfusions and 21% who had received ≥6 transfusions. During the 3-year follow-up period, 55% of patients experienced at least one H-VOC with a median length of stay of 16 (IQR 6–45) days. History of H-VOC was significantly associated with a higher rate of subsequent H-VOC (incidence rate ratio [IRR] 4.32, 95% confidence interval [CI] 2.86 to 6.61, P<0.001) and a longer stay (IRR 5.37, 95% CI 3.00 to 9.77, P<0.001; Table). Transfusion history was also significantly associated with a higher rate of subsequent H-VOC (IRR 1.58, 95% CI 1.05 to 2.38, P=0.030) and a longer stay (IRR 3.79, 95% CI 2.03 to 7.06, P<0.001; Table). However, further analysis to investigate the effect of transfusion frequency (ie chronic versus rescue transfusions) is needed. Secondary analysis, including hospitalized patients only (n=112), found a HbSC or HbSβ-thalassemia genotype, a body mass index of <18.5 kg/m2 (ie underweight), a higher aspartate aminotransferase level and transfusion history were associated with a longer stay. Older age, males, and history of opioid use were associated with a shorter stay (Table).
Conclusion
Our results demonstrate that history of H-VOC within the preceding 12 months was significantly associated with a higher rate of subsequent H-VOC and increased length of stay in our cohort, independently of age, sex and genotype. Our data have limited statistical power and generalizability. Therefore, future studies in larger cohorts and/or different geographical populations are needed. However, in combination with the widely accepted impact that VOCs have on morbidity and mortality, these findings further support the need to reduce/prevent VOCs in SCD patients.
Keyword(s): Clinical outcome, Risk factor, Sickle cell disease
Abstract: EP1222
Type: E-Poster Presentation
Session title: Sickle cell disease
Background
Sickle cell disease (SCD) is a global health burden that has been largely neglected. Despite improvements in diagnosis, treatment and management over the past few decades, SCD morbidity including vaso-occlusive crises (VOCs) remains high. VOCs, the hallmark of SCD, are the primary cause of hospitalization for SCD patients, and are associated with significant morbidity and mortality. Evidence regarding potential risk factors for hospitalization due to VOC (H-VOC) including commonly measured blood markers is limited.
Aims
To assess whether selected factors are associated with the rate of H-VOC and hospital length of stay by performing a retrospective analysis of data collected prospectively during a 3-year, multicenter, observational US study (NCT01220115) that aimed to better understand disease burden and management of SCD in patients aged ≥2 years.
Methods
Out of a total of 498 recruited patients, 202 aged ≥16 years and for whom patient-reported hospital admission data were available were included in this analysis. Negative binomial regression (adjusted for age, sex, and SCD genotype) was used to examine the association of selected baseline characteristics (ie body mass index, hemoglobin, ferritin, transaminases, and any history [received in the preceding 12 months] of opioids, hydroxyurea, transfusion, and H-VOC) with the frequency and length of stay of H-VOC in SCD patients.
Results
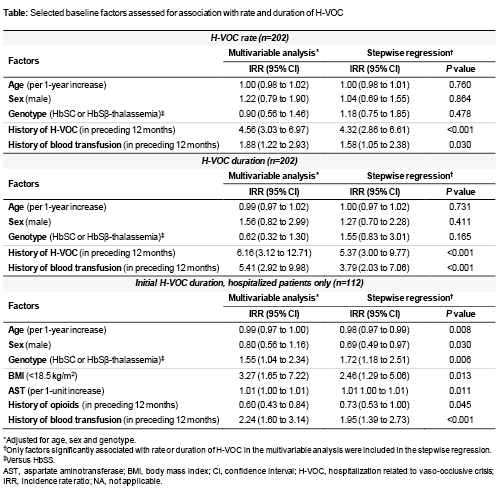
Overall, 71% of patients had a HbSS genotype, 98% were Black or African American and 51% were female. The median age of the cohort was 31 years (interquartile range [IQR] 22–41). At baseline, 36% of patients had received opioids, 14% had received hydroxyurea and 51% had received transfusions in the previous 12 months, comprising 30% who had received 1–5 transfusions and 21% who had received ≥6 transfusions. During the 3-year follow-up period, 55% of patients experienced at least one H-VOC with a median length of stay of 16 (IQR 6–45) days. History of H-VOC was significantly associated with a higher rate of subsequent H-VOC (incidence rate ratio [IRR] 4.32, 95% confidence interval [CI] 2.86 to 6.61, P<0.001) and a longer stay (IRR 5.37, 95% CI 3.00 to 9.77, P<0.001; Table). Transfusion history was also significantly associated with a higher rate of subsequent H-VOC (IRR 1.58, 95% CI 1.05 to 2.38, P=0.030) and a longer stay (IRR 3.79, 95% CI 2.03 to 7.06, P<0.001; Table). However, further analysis to investigate the effect of transfusion frequency (ie chronic versus rescue transfusions) is needed. Secondary analysis, including hospitalized patients only (n=112), found a HbSC or HbSβ-thalassemia genotype, a body mass index of <18.5 kg/m2 (ie underweight), a higher aspartate aminotransferase level and transfusion history were associated with a longer stay. Older age, males, and history of opioid use were associated with a shorter stay (Table).
Conclusion
Our results demonstrate that history of H-VOC within the preceding 12 months was significantly associated with a higher rate of subsequent H-VOC and increased length of stay in our cohort, independently of age, sex and genotype. Our data have limited statistical power and generalizability. Therefore, future studies in larger cohorts and/or different geographical populations are needed. However, in combination with the widely accepted impact that VOCs have on morbidity and mortality, these findings further support the need to reduce/prevent VOCs in SCD patients.
Keyword(s): Clinical outcome, Risk factor, Sickle cell disease


