
Contributions
Abstract: EP1092
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Bone marrow (BM) fibrosis is one of the key histological features of myelofibrosis (MF); high-grade BM fibrosis is associated with worse outcome in patients (pts) with MF. Prefibrotic MF is characterized by low-grade BM fibrosis (0-1) and is described as a separate entity from overt MF in the WHO 2016 classification. Ruxolitinib (RUX) is a potent JAK1/JAK2 inhibitor that has shown improvement of MF-related symptoms and increased overall survival (OS) in pts with MF. The JUMP phase 3b, expanded-access trial (NCT01493414) assessed the safety and efficacy of RUX in pts with symptomatic MF without access to RUX outside of the clinical trial setting (N=2,233).
Aims
To investigate the impact of BM fibrosis grade on response and outcome in pts with primary MF (PMF) treated with RUX.
Methods
Pts ≥18 years (y) with PMF, and with an enlarged spleen (≥5 cm from costal margin) were included in this analysis. BM fibrosis was assessed locally by biopsy and graded 0 to 3. Although the primary endpoint of the study was safety, efficacy of RUX was assessed by secondary endpoints including changes in spleen length by palpation, progression-free survival (PFS), and OS. The present work is a post hoc analysis, and thus was not statistically powered.
Results
A total of 1,326/2,233 pts with PMF had a documented biopsy (grade 0, n=25; grade 1, n=243; grade 2, n=433; grade 3, n=419). The median age at baseline was 67 years (range, 18–89 years). Median time since initial diagnosis was similar between pts with lower grade fibrosis (LGF, grade 0-1; 31.8 months [range, 0.3–296.4]) and higher grade fibrosis (HGF, grade 2-3; 25.5 months [range, 0.1–456.0]). Pts with HGF had more cases of anemia and thrombocytopenia at baseline (HGF vs LGF: 46.4% vs 32.5% pts with hemoglobin <100 g/L; 8.6% vs 4.1% pts with platelets <100 x 109/L). Mean (SD) palpable spleen length (cm below costal margin) at baseline was similar between patient groups (LGF vs HGF: 11.3 [7.1] vs 12.9 [7.2]), as were mean FACIT – Fatigue and FACT – Lymphoma total scores (34.5 and 115.4 for pts with LGF vs 32.8 and 114.9 for pts with HGF, respectively).
A larger proportion of pts with LGF achieved a ≥50% spleen length reduction at week 24 (62.4% vs 55.1% in pts with HGF). Furthermore, a clear trend was observed between grade of fibrosis and spleen response at week 24 (66.7% for grade 0, 62.0% for grade 1, 59.5% for grade 2, and 50.2% for grade 3). Spleen response at week 24 was higher for pts who initiated RUX ≤2 y after diagnosis irrespective of fibrosis grade (64.0% vs 61.1% in >2 y in LGF; 61.5% vs 49.2% in >2 y in HGF).
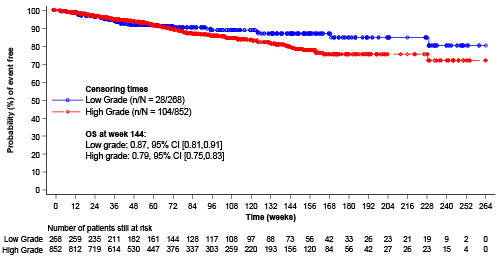
PFS estimates at week 144 were 82% for pts with LGF and 70% for pts with HGF. LGF was associated with higher OS at week 144 (91% for grade 0, 87% for grade 1, 80% for grade 2, and 78% for grade 3). OS probability estimate at week 144 was 87% for pts with LGF (n=73), and 79% for pts with HGF (n=156); median OS was not achieved by either pt group (Figure). More deaths were recorded for pts with LGF who initiated RUX >2 y after diagnosis (death events: 12.4% vs 8.1% for pts ≤2 y); this effect was not observed in pts with HGF (death events: 11.4% vs 13.0% for pts ≤2 y).
Conclusion
PMF symptomatology and splenomegaly are comparable in LGF and HGF pts, suggesting an unmet need in LGF pts. RUX therapy is associated with improved spleen responses and survival in both cohorts, but more so in LGF pts; however, LGF could also be a marker of better clinical characteristics at baseline. Early treatment with RUX may improve clinical benefits for both LGF and HGF pts.
Keyword(s): Bone Marrow Fibrosis, Myelofibrosis, Ruxolitinib
Abstract: EP1092
Type: E-Poster Presentation
Session title: Myeloproliferative neoplasms - Clinical
Background
Bone marrow (BM) fibrosis is one of the key histological features of myelofibrosis (MF); high-grade BM fibrosis is associated with worse outcome in patients (pts) with MF. Prefibrotic MF is characterized by low-grade BM fibrosis (0-1) and is described as a separate entity from overt MF in the WHO 2016 classification. Ruxolitinib (RUX) is a potent JAK1/JAK2 inhibitor that has shown improvement of MF-related symptoms and increased overall survival (OS) in pts with MF. The JUMP phase 3b, expanded-access trial (NCT01493414) assessed the safety and efficacy of RUX in pts with symptomatic MF without access to RUX outside of the clinical trial setting (N=2,233).
Aims
To investigate the impact of BM fibrosis grade on response and outcome in pts with primary MF (PMF) treated with RUX.
Methods
Pts ≥18 years (y) with PMF, and with an enlarged spleen (≥5 cm from costal margin) were included in this analysis. BM fibrosis was assessed locally by biopsy and graded 0 to 3. Although the primary endpoint of the study was safety, efficacy of RUX was assessed by secondary endpoints including changes in spleen length by palpation, progression-free survival (PFS), and OS. The present work is a post hoc analysis, and thus was not statistically powered.
Results
A total of 1,326/2,233 pts with PMF had a documented biopsy (grade 0, n=25; grade 1, n=243; grade 2, n=433; grade 3, n=419). The median age at baseline was 67 years (range, 18–89 years). Median time since initial diagnosis was similar between pts with lower grade fibrosis (LGF, grade 0-1; 31.8 months [range, 0.3–296.4]) and higher grade fibrosis (HGF, grade 2-3; 25.5 months [range, 0.1–456.0]). Pts with HGF had more cases of anemia and thrombocytopenia at baseline (HGF vs LGF: 46.4% vs 32.5% pts with hemoglobin <100 g/L; 8.6% vs 4.1% pts with platelets <100 x 109/L). Mean (SD) palpable spleen length (cm below costal margin) at baseline was similar between patient groups (LGF vs HGF: 11.3 [7.1] vs 12.9 [7.2]), as were mean FACIT – Fatigue and FACT – Lymphoma total scores (34.5 and 115.4 for pts with LGF vs 32.8 and 114.9 for pts with HGF, respectively).
A larger proportion of pts with LGF achieved a ≥50% spleen length reduction at week 24 (62.4% vs 55.1% in pts with HGF). Furthermore, a clear trend was observed between grade of fibrosis and spleen response at week 24 (66.7% for grade 0, 62.0% for grade 1, 59.5% for grade 2, and 50.2% for grade 3). Spleen response at week 24 was higher for pts who initiated RUX ≤2 y after diagnosis irrespective of fibrosis grade (64.0% vs 61.1% in >2 y in LGF; 61.5% vs 49.2% in >2 y in HGF).
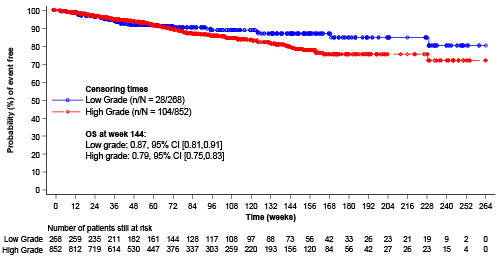
PFS estimates at week 144 were 82% for pts with LGF and 70% for pts with HGF. LGF was associated with higher OS at week 144 (91% for grade 0, 87% for grade 1, 80% for grade 2, and 78% for grade 3). OS probability estimate at week 144 was 87% for pts with LGF (n=73), and 79% for pts with HGF (n=156); median OS was not achieved by either pt group (Figure). More deaths were recorded for pts with LGF who initiated RUX >2 y after diagnosis (death events: 12.4% vs 8.1% for pts ≤2 y); this effect was not observed in pts with HGF (death events: 11.4% vs 13.0% for pts ≤2 y).
Conclusion
PMF symptomatology and splenomegaly are comparable in LGF and HGF pts, suggesting an unmet need in LGF pts. RUX therapy is associated with improved spleen responses and survival in both cohorts, but more so in LGF pts; however, LGF could also be a marker of better clinical characteristics at baseline. Early treatment with RUX may improve clinical benefits for both LGF and HGF pts.
Keyword(s): Bone Marrow Fibrosis, Myelofibrosis, Ruxolitinib


