
Contributions
Abstract: S314
Type: Oral Presentation
Session title: Patient's voice and health outcomes in hematology
Background
SCD is a group of inherited blood disorders associated with a range of clinical complications mainly mediated by vaso-occlusion and hemolytic anemia. Vaso-occlusive crises (VOCs) are the hallmark of SCD, and the most common cause of hospitalization. SCD is a global public health problem, with African countries having the highest disease prevalence.
Aims
To use SWAY data to compare the negative impact of SCD (examining symptoms, complications and quality of life) on patients (pts) in Ghana/Nigeria vs pts in other low-/middle income (LMIC) and high-income countries (HIC). SCD impact stratified by primary care provider (specialist vs non-specialist HCP) was also assessed.
Methods
SWAY was a multicountry survey (Apr–Oct 2019) developed by international SCD experts, pt advocacy groups and Novartis. Pts with SCD ≥6 years old completed the survey (completion by proxy [parent/guardian/caregiver] was required for pts aged 6–11 years, optional for pts ≥12 years). The World Bank definition of an HI economy (gross national income/capita ≥US$12,536) was used to stratify countries into LMIC and HIC. VOCs (defined as ‘severe pain crises’), symptoms (experienced in the month preceding survey completion [excluding VOCs]), complications (ever experienced) and genotype were all self-reported. Responses to questions on the impact of SCD were classified on a 1–7 Likert scale (1=not severe/strongly disagree, 7=worst imaginable/strongly agree; with 5–7 indicating high impact/agreement). Pt participants (N=2145) were grouped into Ghana/Nigeria (n=519), other LMIC (Brazil, India, Lebanon [n=422]) and HIC (Bahrain, Canada, France, Germany, Italy, Netherlands, Oman, Panama, Saudi Arabia, USA, UK [n=1204]).
Results
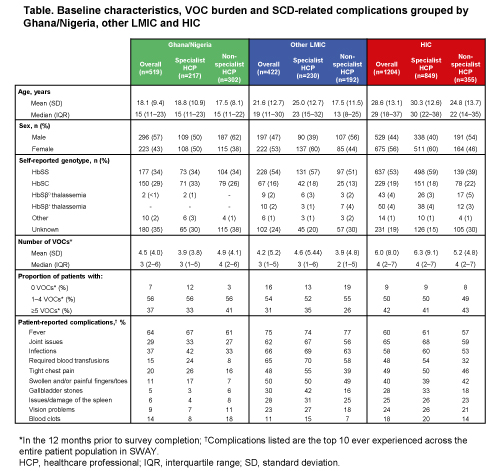
Pts in Ghana/Nigeria were younger than those in other LMIC/HIC, and the mean number of VOCs experienced in the year before survey completion was lower in Ghana/Nigeria (4.5) and other LMIC (4.2) vs HIC (6.0) (Table). The top 3 most commonly reported symptoms in the month preceding survey were headache (Ghana/Nigeria 58%; LMIC 39%; HIC 44%), fatigue (Ghana/Nigeria 34%; LMIC 69%; HIC 77%) and bone aches (Ghana/Nigeria 32%; LMIC 56%; HIC 58%). Of the top 10 most frequently reported complications, all (except blood clots and fever) were reported by a lower proportion of pts in Ghana/Nigeria vs pts in other LMIC/HIC (Table). In Ghana/Nigeria, pts treated by a non-specialist HCP generally reported greater symptom prevalence than those treated by a specialist HCP. In contrast, the proportion of pts in other LMIC reporting symptoms was higher in the specialist HCP-treated group for most symptoms assessed. Pts in Ghana/Nigeria reported a lower or similar use of analgesics compared with other LMIC/HIC, with 26% ever prescribed opioids (other LMIC 28%; HIC 73%) and 30% ever receiving OTC analgesics (LMIC 63%; HIC 64%). In Ghana/Nigeria, 52% of pts reported that SCD had a high negative impact on their emotional wellbeing vs 56% of pts in other LMIC and 64% in HIC.
Conclusion
The reported overall burden of SCD appeared to be lower on pts in Ghana/Nigeria than for those in other LMIC/HIC. A possible explanation for this is the younger age of pts from Ghana/Nigeria, where a high infant mortality rate means many pts do not live long enough to develop chronic complications. Other explanations may include limited availability of resources to detect symptoms/complications, warmer climate, low usage of analgesics and poor education for both pts (and, potentially, non-specialist HCPs) in Ghana/Nigeria vs other countries participating in SWAY.
Keyword(s): Quality of life, Sickle cell disease, Sickle cell patient, Vasoocclusive crisis
Abstract: S314
Type: Oral Presentation
Session title: Patient's voice and health outcomes in hematology
Background
SCD is a group of inherited blood disorders associated with a range of clinical complications mainly mediated by vaso-occlusion and hemolytic anemia. Vaso-occlusive crises (VOCs) are the hallmark of SCD, and the most common cause of hospitalization. SCD is a global public health problem, with African countries having the highest disease prevalence.
Aims
To use SWAY data to compare the negative impact of SCD (examining symptoms, complications and quality of life) on patients (pts) in Ghana/Nigeria vs pts in other low-/middle income (LMIC) and high-income countries (HIC). SCD impact stratified by primary care provider (specialist vs non-specialist HCP) was also assessed.
Methods
SWAY was a multicountry survey (Apr–Oct 2019) developed by international SCD experts, pt advocacy groups and Novartis. Pts with SCD ≥6 years old completed the survey (completion by proxy [parent/guardian/caregiver] was required for pts aged 6–11 years, optional for pts ≥12 years). The World Bank definition of an HI economy (gross national income/capita ≥US$12,536) was used to stratify countries into LMIC and HIC. VOCs (defined as ‘severe pain crises’), symptoms (experienced in the month preceding survey completion [excluding VOCs]), complications (ever experienced) and genotype were all self-reported. Responses to questions on the impact of SCD were classified on a 1–7 Likert scale (1=not severe/strongly disagree, 7=worst imaginable/strongly agree; with 5–7 indicating high impact/agreement). Pt participants (N=2145) were grouped into Ghana/Nigeria (n=519), other LMIC (Brazil, India, Lebanon [n=422]) and HIC (Bahrain, Canada, France, Germany, Italy, Netherlands, Oman, Panama, Saudi Arabia, USA, UK [n=1204]).
Results
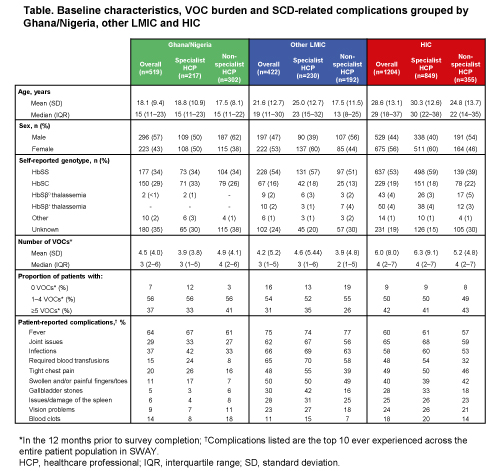
Pts in Ghana/Nigeria were younger than those in other LMIC/HIC, and the mean number of VOCs experienced in the year before survey completion was lower in Ghana/Nigeria (4.5) and other LMIC (4.2) vs HIC (6.0) (Table). The top 3 most commonly reported symptoms in the month preceding survey were headache (Ghana/Nigeria 58%; LMIC 39%; HIC 44%), fatigue (Ghana/Nigeria 34%; LMIC 69%; HIC 77%) and bone aches (Ghana/Nigeria 32%; LMIC 56%; HIC 58%). Of the top 10 most frequently reported complications, all (except blood clots and fever) were reported by a lower proportion of pts in Ghana/Nigeria vs pts in other LMIC/HIC (Table). In Ghana/Nigeria, pts treated by a non-specialist HCP generally reported greater symptom prevalence than those treated by a specialist HCP. In contrast, the proportion of pts in other LMIC reporting symptoms was higher in the specialist HCP-treated group for most symptoms assessed. Pts in Ghana/Nigeria reported a lower or similar use of analgesics compared with other LMIC/HIC, with 26% ever prescribed opioids (other LMIC 28%; HIC 73%) and 30% ever receiving OTC analgesics (LMIC 63%; HIC 64%). In Ghana/Nigeria, 52% of pts reported that SCD had a high negative impact on their emotional wellbeing vs 56% of pts in other LMIC and 64% in HIC.
Conclusion
The reported overall burden of SCD appeared to be lower on pts in Ghana/Nigeria than for those in other LMIC/HIC. A possible explanation for this is the younger age of pts from Ghana/Nigeria, where a high infant mortality rate means many pts do not live long enough to develop chronic complications. Other explanations may include limited availability of resources to detect symptoms/complications, warmer climate, low usage of analgesics and poor education for both pts (and, potentially, non-specialist HCPs) in Ghana/Nigeria vs other countries participating in SWAY.
Keyword(s): Quality of life, Sickle cell disease, Sickle cell patient, Vasoocclusive crisis


