
Contributions
Abstract: S296
Type: Oral Presentation
Session title: ITP: from bench to bedside
Background
Immune thrombocytopenia (ITP) exists in a primary form with no underlying cause (pITP), and a secondary form (sITP). Survival in pITP has been found to be reduced compared to background populations. However, only few studies on long-term outcomes and prognosis have been conducted, and prognosis of sITP is to our knowledge unknown.
Aims
In this study, we leverage the unique Danish patient registries to present long-term survival for patients with chronic primary and secondary immune thrombocytopenia.
Methods
Incident chronic ITP patients aged ≥ 18 years were identified as patients with two defined WHO ICD-8 or ICD-10 ITP-diagnosis codes registrations ≥ 12 months apart in any Danish hospital during 1980-2016. Patients with prevalent ITP at the beginning of the study period were excluded (using data from 1977-1979).
Among patients with chronic ITP, sITP cases were identified using the designated ICD10-code (D695) or through registration of an associated diagnosis before or up to 12 months after the first ITP diagnosis.
For each ITP patient, we identified and matched up to 50 individuals from the background population and not previously registered with ITP, matching on age and sex. Patients’ index date were the date of the second diagnosis registration after ≥ 12 months, assigning comparison individuals an index date corresponding to the matched ITP patient. Individuals were followed from index date until death, emigration, or end of study, whichever came first.
Results
We identified 3,402 patients fulfilling primary criteria for chronic ITP. Of these, 836 were excluded (210 were prevalent, 506 were <18years of age, 80 had congenital platelet disorders and 40 had Evans syndrome) yielding a total of 2,566 patients with chronic ITP in the period 1980-2016. Comparisons comprised 123,244 individuals.
Among patients with chronic ITP 90.3% (n=2,318) were classified as pITP and 9.7% (n=248) as sITP (associated diagnoses were immunodeficiency (<5), autoimmunity (n=119), infection (n=46), hematological cancer (n=48) or D695 ICD-code only (n=48), with some overlap between groups).
The entire cohort included 60.3% women and mean age at index date was 55.5 [95% CI: 55.4; 55.6], 19.9% (n=511) of all patients with chronic ITP and 0.2% (n=251) of all comparisons were splenectomized.
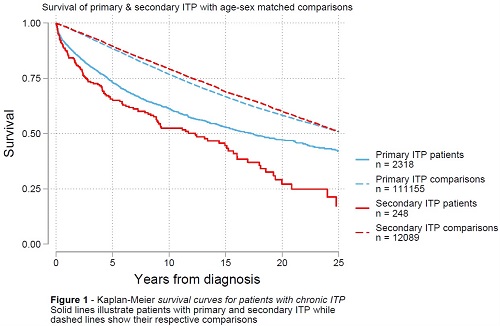
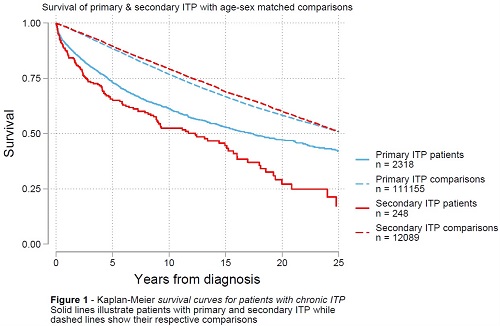
Survival analysis showed that median survival [95%CI] was 17.3 years [15.3; 20.0] for patients with pITP and 25.5 years [25.2; 26.0] for their corresponding comparisons. For patients with sITP, median survival was reduced to 12.3 years [8.9; 15.2], and 25.8 years [24.6; 27.1] for their comparisons (Figure 1).
When performing Cox-regression, hazard ratio (HR) for death between groups was 1.85 [1.74; 1.97] when comparing all patients with chronic ITP to all comparisons (total number of comparisons in the cohort). Risk of death for patients with sITP vs. pITP (adjusted for age) was also elevated with a HR of 1.50 [1.24; 1.81].
Subgroup analyses for both pITP and sITP vs. respective comparisons were also performed. For patients with pITP vs. comparisons HR was 1.77 [1.66; 1.89], and among patients with sITP vs. comparisons HR was 2.79 [2.33; 3.33].
Conclusion
Survival for both pITP and sITP are reduced compared to the general population.
This cohort provides a unique possibility of future outcome studies of patients with pITP and sITP.
Analyses of temporal trends and comorbidity are ongoing and will be presented with the abstract.
Keyword(s): Epidemiology, Immune thrombocytopenia (ITP), Outcome measurement, Survival
Abstract: S296
Type: Oral Presentation
Session title: ITP: from bench to bedside
Background
Immune thrombocytopenia (ITP) exists in a primary form with no underlying cause (pITP), and a secondary form (sITP). Survival in pITP has been found to be reduced compared to background populations. However, only few studies on long-term outcomes and prognosis have been conducted, and prognosis of sITP is to our knowledge unknown.
Aims
In this study, we leverage the unique Danish patient registries to present long-term survival for patients with chronic primary and secondary immune thrombocytopenia.
Methods
Incident chronic ITP patients aged ≥ 18 years were identified as patients with two defined WHO ICD-8 or ICD-10 ITP-diagnosis codes registrations ≥ 12 months apart in any Danish hospital during 1980-2016. Patients with prevalent ITP at the beginning of the study period were excluded (using data from 1977-1979).
Among patients with chronic ITP, sITP cases were identified using the designated ICD10-code (D695) or through registration of an associated diagnosis before or up to 12 months after the first ITP diagnosis.
For each ITP patient, we identified and matched up to 50 individuals from the background population and not previously registered with ITP, matching on age and sex. Patients’ index date were the date of the second diagnosis registration after ≥ 12 months, assigning comparison individuals an index date corresponding to the matched ITP patient. Individuals were followed from index date until death, emigration, or end of study, whichever came first.
Results
We identified 3,402 patients fulfilling primary criteria for chronic ITP. Of these, 836 were excluded (210 were prevalent, 506 were <18years of age, 80 had congenital platelet disorders and 40 had Evans syndrome) yielding a total of 2,566 patients with chronic ITP in the period 1980-2016. Comparisons comprised 123,244 individuals.
Among patients with chronic ITP 90.3% (n=2,318) were classified as pITP and 9.7% (n=248) as sITP (associated diagnoses were immunodeficiency (<5), autoimmunity (n=119), infection (n=46), hematological cancer (n=48) or D695 ICD-code only (n=48), with some overlap between groups).
The entire cohort included 60.3% women and mean age at index date was 55.5 [95% CI: 55.4; 55.6], 19.9% (n=511) of all patients with chronic ITP and 0.2% (n=251) of all comparisons were splenectomized.
Survival analysis showed that median survival [95%CI] was 17.3 years [15.3; 20.0] for patients with pITP and 25.5 years [25.2; 26.0] for their corresponding comparisons. For patients with sITP, median survival was reduced to 12.3 years [8.9; 15.2], and 25.8 years [24.6; 27.1] for their comparisons (Figure 1).
When performing Cox-regression, hazard ratio (HR) for death between groups was 1.85 [1.74; 1.97] when comparing all patients with chronic ITP to all comparisons (total number of comparisons in the cohort). Risk of death for patients with sITP vs. pITP (adjusted for age) was also elevated with a HR of 1.50 [1.24; 1.81].
Subgroup analyses for both pITP and sITP vs. respective comparisons were also performed. For patients with pITP vs. comparisons HR was 1.77 [1.66; 1.89], and among patients with sITP vs. comparisons HR was 2.79 [2.33; 3.33].
Conclusion
Survival for both pITP and sITP are reduced compared to the general population.
This cohort provides a unique possibility of future outcome studies of patients with pITP and sITP.
Analyses of temporal trends and comorbidity are ongoing and will be presented with the abstract.
Keyword(s): Epidemiology, Immune thrombocytopenia (ITP), Outcome measurement, Survival


