
Contributions
Abstract: PB2360
Type: Publication Only
Background
In our practice we have observed a number of patients with immune thrombocytopenia (ITP) whose platelet count has increased after vitamin D replacement alone, prompting us to investigate this further. Vitamin D deficiency has been linked with the development of autoimmune disease. This pathophysiological mechanism may also apply to patients with ITP, in which case, correcting vitamin D deficiency would be a safe way of aiding treatment.
Aims
Assess whether there is a relationship between ITP and vitamin D deficiency in both adults and children.
Methods
Adult and pediatric ITP patient cohorts were retrospectively analysed, comprising of 148 and 34 patients respectively. The pediatric cohort was further divided into acute (11) and chronic (23) groups. Vitamin D laboratory tests were reviewed and classified as – replete (>70nmol/L), insufficient (40 – 70nmol/L) or deficient (<40nmol/L). Platelet counts taken at the same time as vitamin D testing were also recorded. Thrombocytopenias were categorised as mild (>30x109/L), moderate (10-30x109/L) or severe (<10x109/L). Those with repeat vitamin D tests were categorised as – increased, unchanged or decreased vitamin D level, based on category (replete, insufficient or deficient) rather than numerical value.
Results
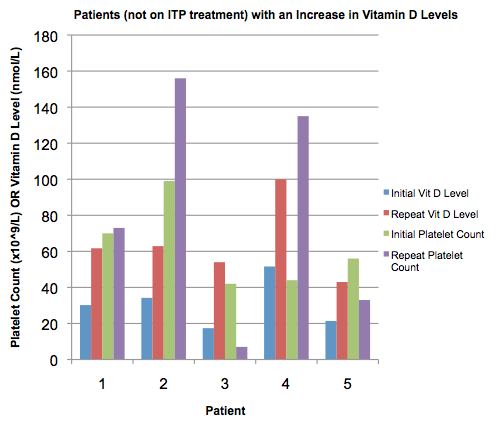
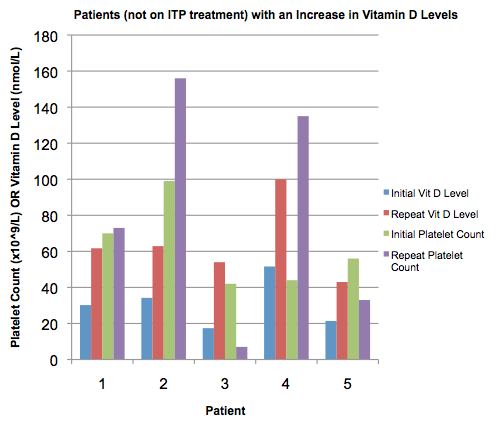
In the pediatric chronic ITP group, of the 20 patients tested, the mean vitamin D level was 46.4nmol/L (SD ±25.8). 40% of these were deficient and 35% insufficient. In the acute ITP group 6 patients were tested, the mean vitamin D level was 47.5 nmol/L (SD ±29.6). Overall, 83.3% of those tested were either deficient or insufficient and this did not correlate with severity of thrombocytopenia. In the adult cohort of 148 patients, 117 (mean age 45 years) had vitamin D levels and platelet counts tested. The mean level was 53.8nmol/L (SD ±31.7). Of these, 35% were deficient, 41% insufficient and 24% replete. When stratified by severity of thrombocytopenia, there was no significant difference between groups. There were significantly more patients deficient in winter and spring compared to in summer and autumn. Plotting numerical values of vitamin D level against platelet count showed little correlation, with a Pearson R value of -0.0048. 47 patients underwent repeat testing for vitamin D levels. Vitamin D levels increased in 17, remained unchanged in 24 and decreased in 6 patients. When stratified by change in platelet count (by category, rather than numerical value), 5 patients showed an increase in both vitamin D and platelet count, 2 of which were on no other treatment for ITP. This was not a consistent change with others having a fall in platelet count despite an increase in vitamin D levels.
Conclusion
From our data, a small number of patients had an increase in their platelet count with vitamin D replacement alone. However, this was not a consistent effect and there was no overall correlation between vitamin D deficiency and thrombocytopenia. Nonetheless, this is a heterogeneous group of patients, on a variety of treatments which were not accounted for. Vitamin D deficiency is a significant problem in our cohort of children and adults with ITP. Vitamin D is of clear importance in regulation of the immune system with an apparent protective effect against infections. The role of vitamin D in autoimmune conditions is harder to establish given the heterogeneity of disease and the variability of clinical trials performed in this area. However, given the low sunlight in the UK and the importance of vitamin D for overall immunity, we recommend testing for and replacing vitamin D, particularly over winter months.
Session topic: 33. Platelets disorders
Keyword(s): Immune thrombocytopenia (ITP)
Abstract: PB2360
Type: Publication Only
Background
In our practice we have observed a number of patients with immune thrombocytopenia (ITP) whose platelet count has increased after vitamin D replacement alone, prompting us to investigate this further. Vitamin D deficiency has been linked with the development of autoimmune disease. This pathophysiological mechanism may also apply to patients with ITP, in which case, correcting vitamin D deficiency would be a safe way of aiding treatment.
Aims
Assess whether there is a relationship between ITP and vitamin D deficiency in both adults and children.
Methods
Adult and pediatric ITP patient cohorts were retrospectively analysed, comprising of 148 and 34 patients respectively. The pediatric cohort was further divided into acute (11) and chronic (23) groups. Vitamin D laboratory tests were reviewed and classified as – replete (>70nmol/L), insufficient (40 – 70nmol/L) or deficient (<40nmol/L). Platelet counts taken at the same time as vitamin D testing were also recorded. Thrombocytopenias were categorised as mild (>30x109/L), moderate (10-30x109/L) or severe (<10x109/L). Those with repeat vitamin D tests were categorised as – increased, unchanged or decreased vitamin D level, based on category (replete, insufficient or deficient) rather than numerical value.
Results
In the pediatric chronic ITP group, of the 20 patients tested, the mean vitamin D level was 46.4nmol/L (SD ±25.8). 40% of these were deficient and 35% insufficient. In the acute ITP group 6 patients were tested, the mean vitamin D level was 47.5 nmol/L (SD ±29.6). Overall, 83.3% of those tested were either deficient or insufficient and this did not correlate with severity of thrombocytopenia. In the adult cohort of 148 patients, 117 (mean age 45 years) had vitamin D levels and platelet counts tested. The mean level was 53.8nmol/L (SD ±31.7). Of these, 35% were deficient, 41% insufficient and 24% replete. When stratified by severity of thrombocytopenia, there was no significant difference between groups. There were significantly more patients deficient in winter and spring compared to in summer and autumn. Plotting numerical values of vitamin D level against platelet count showed little correlation, with a Pearson R value of -0.0048. 47 patients underwent repeat testing for vitamin D levels. Vitamin D levels increased in 17, remained unchanged in 24 and decreased in 6 patients. When stratified by change in platelet count (by category, rather than numerical value), 5 patients showed an increase in both vitamin D and platelet count, 2 of which were on no other treatment for ITP. This was not a consistent change with others having a fall in platelet count despite an increase in vitamin D levels.
Conclusion
From our data, a small number of patients had an increase in their platelet count with vitamin D replacement alone. However, this was not a consistent effect and there was no overall correlation between vitamin D deficiency and thrombocytopenia. Nonetheless, this is a heterogeneous group of patients, on a variety of treatments which were not accounted for. Vitamin D deficiency is a significant problem in our cohort of children and adults with ITP. Vitamin D is of clear importance in regulation of the immune system with an apparent protective effect against infections. The role of vitamin D in autoimmune conditions is harder to establish given the heterogeneity of disease and the variability of clinical trials performed in this area. However, given the low sunlight in the UK and the importance of vitamin D for overall immunity, we recommend testing for and replacing vitamin D, particularly over winter months.
Session topic: 33. Platelets disorders
Keyword(s): Immune thrombocytopenia (ITP)


